How Autoimmune Disorders Trigger Alopecia: Causes, Types & Treatment
Autoimmune Disorder & Alopecia Link Checker
Common Autoimmune Disorders Linked to Alopecia
Hashimoto's Thyroiditis
Causes diffuse thinning due to hypothyroidism.
Fatigue Weight gain Cold intoleranceGraves' Disease
Can cause both diffuse and patchy hair loss.
Heat intolerance Tremor Bulging eyesSystemic Lupus Erythematosus
May present as alopecia areata-like patches.
Butterfly rash Joint pain Kidney issuesVitiligo
Results in localized bald spots with depigmented skin.
White patches Hair lossCeliac Disease
Causes diffuse thinning due to nutrient deficiency.
Abdominal pain Bloating AnemiaPsoriasis
Can lead to psoriatic alopecia on scalp.
Red scaly patches ItchingType 1 Diabetes
May cause diffuse thinning, especially on scalp.
Elevated blood sugar Frequent urinationDid you know that up to 30% of people with alopecia have an underlying autoimmune condition? That statistic flips the script on hair loss - it’s often not just a cosmetic issue but a signal from the immune system.
What Are Autoimmune Disorders?
Autoimmune disease is a condition where the immune system mistakenly attacks the body’s own tissues. Common examples include thyroid disease, lupus, and celiac disease. Instead of defending against germs, the immune cells launch an internal war, causing inflammation, tissue damage, and a host of symptoms that vary wildly from joint pain to digestive trouble.
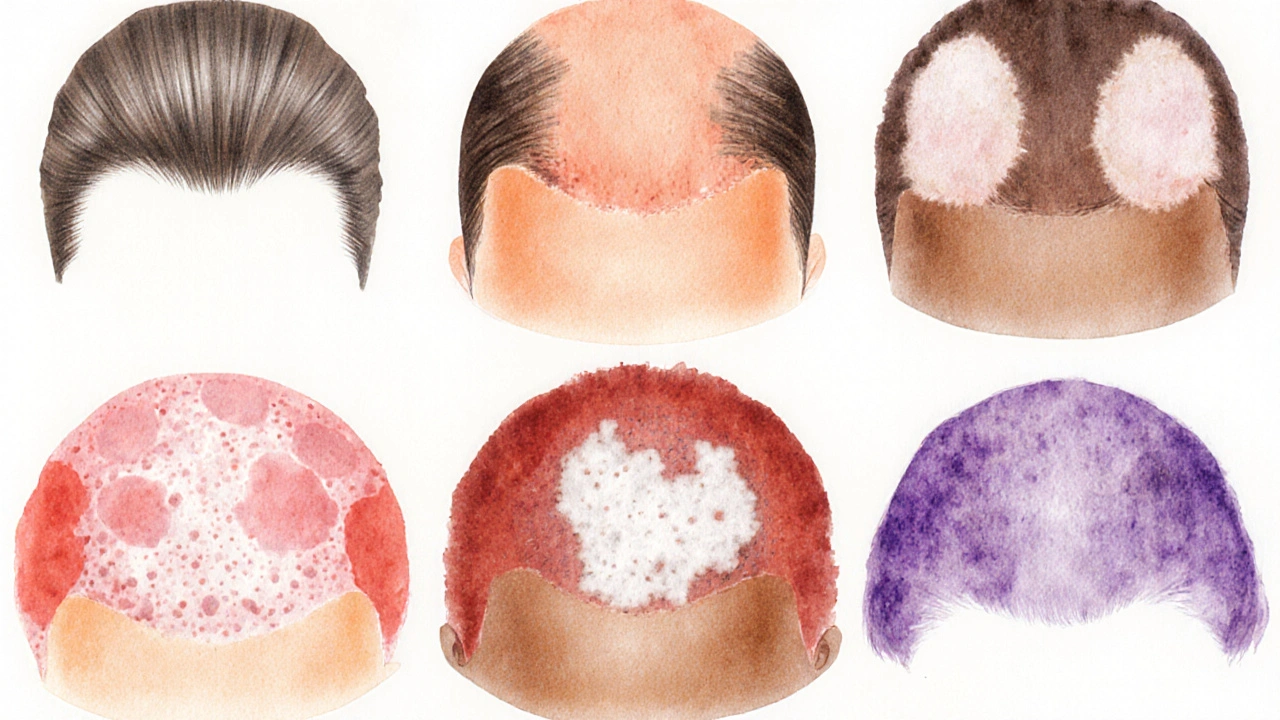
Understanding Alopecia
Alopecia is the medical term for hair loss. It comes in several forms, but the one most linked to autoimmunity is alopecia areata, where round patches of hair vanish suddenly. While anyone can develop alopecia, the immune‑driven variants often have a systemic trigger.
Why the Immune System Targets Hair Follicles
Hair follicles are rich in immune‑privileged cells, meaning they normally hide from immune surveillance. In autoimmune disorders, this shield breaks down. T‑cells, the body’s attack soldiers, start spotting follicle proteins as foreign and launch an assault. The result: inflammation that pushes follicles into a premature resting phase, leading to hair shedding.
Autoimmune Disorders Most Frequently Linked to Alopecia
Below is a snapshot of the conditions that research shows have the strongest correlation with hair loss. Each disorder can provoke a distinct alopecia pattern, from patchy circles to diffuse thinning.
| Disorder | Typical Alopecia Type | Prevalence (Global) | Key Symptoms | Common Treatment Approach |
|---|---|---|---|---|
| Hashimoto's thyroiditis | Diffuse thinning | ~2% of population | Fatigue, weight gain, cold intolerance | Levothyroxine + topical minoxidil |
| Graves' disease | Diffuse or patchy loss | ~0.5% | Heat intolerance, tremor, bulging eyes | Antithyroid meds, radioiodine, steroids |
| Systemic lupus erythematosus (SLE) | Alopecia areata‑like patches | ~0.03% | Butterfly rash, joint pain, kidney issues | Hydroxychloroquine, steroids, immunosuppressants |
| Vitiligo | Localized bald spots with depigmented skin | ~1% | White patches on skin, sometimes hair loss | Topical steroids, phototherapy |
| Celiac disease | Diffuse thinning | ~1% (often undiagnosed) | Abdominal pain, bloating, anemia | Gluten‑free diet, nutritional supplements |
| Psoriasis | Psoriatic alopecia (scalp plaques) | ~2-3% | Red scaly patches, itching | Biologics, topical vitamin D analogues |
| Type 1 diabetes | Diffuse thinning, especially on scalp | ~0.5% | Elevated blood sugar, frequent urination | Insulin therapy, tight glucose control |
Diagnosing the Connection
When you notice sudden hair loss, a dermatologist will first confirm the alopecia pattern with a scalp exam and possibly a pull test. If an autoimmune cause is suspected, they’ll order blood work that may include:
- Thyroid panel (TSH, Free T4)
- ANA (antinuclear antibody) screen for lupus
- Anti‑tissue transglutaminase (tTG) antibodies for celiac disease
- Specific auto‑antibodies for vitiligo or psoriasis
Positive results don’t automatically mean your hair loss is immune‑driven, but they provide a roadmap for targeted therapy.
Managing autoimmune alopecia: Medical Options
Once the underlying disorder is identified, treatment typically follows two tracks: controlling the systemic disease and promoting hair regrowth.
- Immunosuppressants - Corticosteroids (topical or oral) calm the immune flare. For chronic cases, doctors might prescribe methotrexate or azathioprine.
- Biologic agents - Drugs like adalimumab (used for psoriasis) or rituximab (used for lupus) have shown success in stubborn alopecia.
- Topical therapies - Minoxidil 5% solution or foam can stimulate follicles, especially when paired with systemic treatment.
- Hormone modulation - In thyroid‑related hair loss, restoring euthyroid status often restores normal hair cycles within 3-6 months.
It’s crucial to have a multidisciplinary team-dermatology, endocrinology, and sometimes rheumatology-to tailor a regimen that balances efficacy and side‑effects.
Lifestyle Strategies That Support Hair Recovery
Even the best medication can falter if lifestyle factors keep the immune system on edge.
- Nutrition - Adequate protein, iron, zinc, and vitamin D are essential. Many autoimmune patients benefit from a Mediterranean‑style diet rich in omega‑3 fatty acids.
- Stress management - Chronic stress spikes cortisol, which can aggravate both autoimmunity and hair‑cycle disruption. Mindfulness, yoga, or simple breathing exercises have measurable benefits.
- Sleep hygiene - Aim for 7-9 hours of deep sleep. Growth hormone peaks during night‑time, supporting follicle regeneration.
- Avoid harsh hair care - Limit heat styling, tight ponytails, and chemical treatments that can add mechanical stress to already vulnerable follicles.
Tracking progress with photos every 4-6 weeks helps you see subtle regrowth and adjust treatments before problems become entrenched.
When to Seek Professional Help
If you notice any of the following, schedule a dermatologist or primary‑care visit promptly:
- Patchy hair loss lasting more than 2 weeks
- Associated skin changes (redness, depigmentation)
- Systemic symptoms like fatigue, joint pain, or digestive upset
- Rapid shedding across the entire scalp
Early intervention often means a shorter course of high‑dose steroids and a better chance of full regrowth.
Frequently Asked Questions
Can alopecia be the first sign of an autoimmune disease?
Yes. In many cases, especially with alopecia areata, the hair loss shows up before other systemic symptoms. That’s why doctors often run a basic autoimmune panel when someone presents with unexplained patchy hair loss.
Is hair loss reversible once the autoimmune condition is treated?
In most patients, restoring normal immune balance allows follicles to re‑enter the growth phase. Regrowth can take 3-12 months, depending on age, disease severity, and how quickly treatment starts.
Do supplements help with autoimmune‑related hair loss?
Supplements that correct deficiencies-iron, zinc, vitamin D, biotin-can support hair health, but they don’t replace medical therapy. Always test levels before adding high‑dose supplements.
Are there any non‑pharmaceutical treatments proven to work?
Low‑level laser therapy (LLLT) and platelet‑rich plasma (PRP) injections have shown modest benefits in clinical trials, especially when combined with systemic control of the autoimmune disease.
Can lifestyle changes alone cure autoimmune alopecia?
Lifestyle tweaks are powerful adjuncts but rarely cure the condition on their own. They can reduce flare frequency and enhance the effectiveness of medical treatments.
Understanding the link between your immune system and your scalp turns hair loss from a mystery into a manageable health issue. With the right labs, targeted therapy, and daily habits that calm inflammation, many people see their hair grow back-sometimes even stronger than before.

Hang in there you got this!
It is noteworthy that the interplay between systemic autoimmunity and follicular immune privilege warrants meticulous examination. While the article enumerates several disorders, a deeper discussion of the cytokine milieu-particularly interferon‑γ and IL‑17-could enhance mechanistic clarity. Moreover, longitudinal cohort data would substantiate the temporal relationship between disease onset and alopecia manifestation. Such elaborations would render the piece more robust for academic readership.
Honestly this write‑up feels like a sloppy collage of buzzwords masquerading as science; the author neglects to cite primary literature and merely glues together textbook definitions. It reads more like a commercial pamphlet than a credible medical overview.
The pathophysiological nexus between Th1/Th17 skewed responses and follicular keratinocyte apoptosis is a pivotal axis that underpins autoimmune‑induced alopecia. In Hashimoto’s, elevated anti‑thyroid peroxidase antibodies precipitate a cascade of oxidative stressors, culminating in perifollicular inflammation. Conversely, in psoriasis, IL‑23‑driven keratinocyte hyperproliferation establishes psoriatic plaques that can occlude follicular ostia, thereby precipitating scarring alopecia. Integrative omics profiling could elucidate shared transcriptomic signatures across these entities.
Sean, whilst your exposition is undeniably erudite, I must interject: the term “Th1/Th17 skewed responses” should be hyphenated as “Th1/Th17‑skewed responses”; likewise, “anti‑thyroid peroxidase antibodies” benefits from an en‑dash for clarity. Precision in punctuation augments readability; consider revising accordingly.
Lawrence, thanks for the nit‑picky edit-though I think we can both agree the science shines brighter than any stray dash! Let’s keep the focus on helping folks untangle their hair loss mysteries, dash or no dash.
What they don’t tell you is that the pharma giants have a vested interest in keeping alopecia “unsolvable” so they can push pricey biologics. The “autoimmune link” is just a smokescreen to expand their market share while the real cause-environmental toxins-is swept under the rug.
First off, kudos for diving into this complex topic-many shy away from the immunology because it feels intimidating. If you’re wrestling with sudden patchy loss, start with a basic thyroid panel; TSH and free T4 are cheap and often reveal subclinical hypothyroidism that can be treated quickly. Next, consider checking iron studies; anemia can masquerade as diffuse thinning, and iron repletion often yields noticeable regrowth within a few months. Don’t overlook vitamin D-deficiency is rampant in autoimmune cohorts, and supplementation can modulate the immune response. Finally, keep a symptom diary; noting flare‑ups alongside stressors, diet changes, or medication adjustments can help pinpoint triggers that you can then address. Stay persistent, and remember that many patients see meaningful regrowth with the right combo of labs, meds, and lifestyle tweaks.
Marisa, while your pep talk is nice.the real issue is that many patients ignore the underlying dysregulation of the JAK‑STAT pathway, which is why JAK inhibitors have emerged as game‑changers for refractory alopecia.
💡Fun fact: studies show that up to 30% of alopecia patients have elevated anti‑nuclear antibodies, even if they don’t meet full SLE criteria. 🚀 This underscores the importance of a broad autoimmune screen when hair loss is unexplained.
The article exhibits a notable paucity of statistical rigor; without confidence intervals or effect size metrics, the purported associations remain anecdotal. Moreover, the omission of a systematic review methodology undermines its evidentiary weight, relegating it to a narrative editorial rather than a scholarly synthesis.
Adam, nice try sounding all high‑falutin but you’re missing the forest for the trees-people just want clear take‑aways, not a dissertation on p‑values.
Hey everyone, I wanted to share a few thoughts that might help us all feel a bit less overwhelmed by the whole autoimmune‑alopecia maze. First, remember that a diagnosis is just a starting line, not a life sentence; many patients experience remission once the right therapeutic balance is struck. Second, nutrition is a cornerstone-think of your body as a garden, and the nutrients you feed it as the soil; iron, zinc, selenium, and vitamin D are especially crucial for follicular health. Third, stress management isn’t a buzzword; chronic cortisol elevation can sabotage even the best‑planned treatment regimens, so incorporate mindfulness or gentle exercise into your routine. Fourth, keep an eye on medication side effects-some immunosuppressants can paradoxically worsen hair loss if dosages aren’t titrated properly. Fifth, regular lab monitoring is vital; a quarterly thyroid panel, CBC, and inflammatory markers like CRP can catch subtle shifts before they manifest as visible shedding. Sixth, don’t underestimate the power of community-online support groups provide emotional buoyancy and practical tips that clinicians might overlook. Seventh, consider adjunctive therapies such as low‑level laser devices or platelet‑rich plasma; while not miracle cures, they can enhance regrowth when combined with systemic control. Eighth, give your scalp some love: gentle, sulfate‑free shampoos and occasional scalp massages boost local circulation. Ninth, track your progress with photos taken under consistent lighting; this objective record can reveal incremental improvements that your eyes might miss day‑to‑day. Finally, stay patient and compassionate with yourself; hair cycles are slow, and breakthroughs often arrive after months of diligent care. Keep pushing forward, and you’ll likely see those strands make a comeback-sometimes stronger than before.
Look, the way they push pricey patches of medication is no accident; the “cure” they sell is a way to keep us paying forever while the real fix stays hidden.
Oh, absolutely, because the secret sauce to hair growth is definitely locked behind a vault of corporate greed 😒. Maybe if we all chant “free the follicles” the big pharma will finally listen.
Wow, that hits close to home 😢. I’ve watched friends battle the same cycle of hope and disappointment, and it’s heartbreaking. Sending love and virtual hugs to everyone dealing with this.
While the immunological cascade involving cytokine release can appear daunting, it is essential to remember that therapeutic modulation-whether via biologics targeting IL‑6 or small‑molecule JAK inhibitors-offers tangible pathways to restore follicular equilibrium. By integrating these modalities with lifestyle optimization, patients can achieve meaningful regrowth.
Great rundown, everyone-just a heads‑up: “autoimmune alopecia” should be hyphenated as “autoimmune‑alopecia” for consistency.