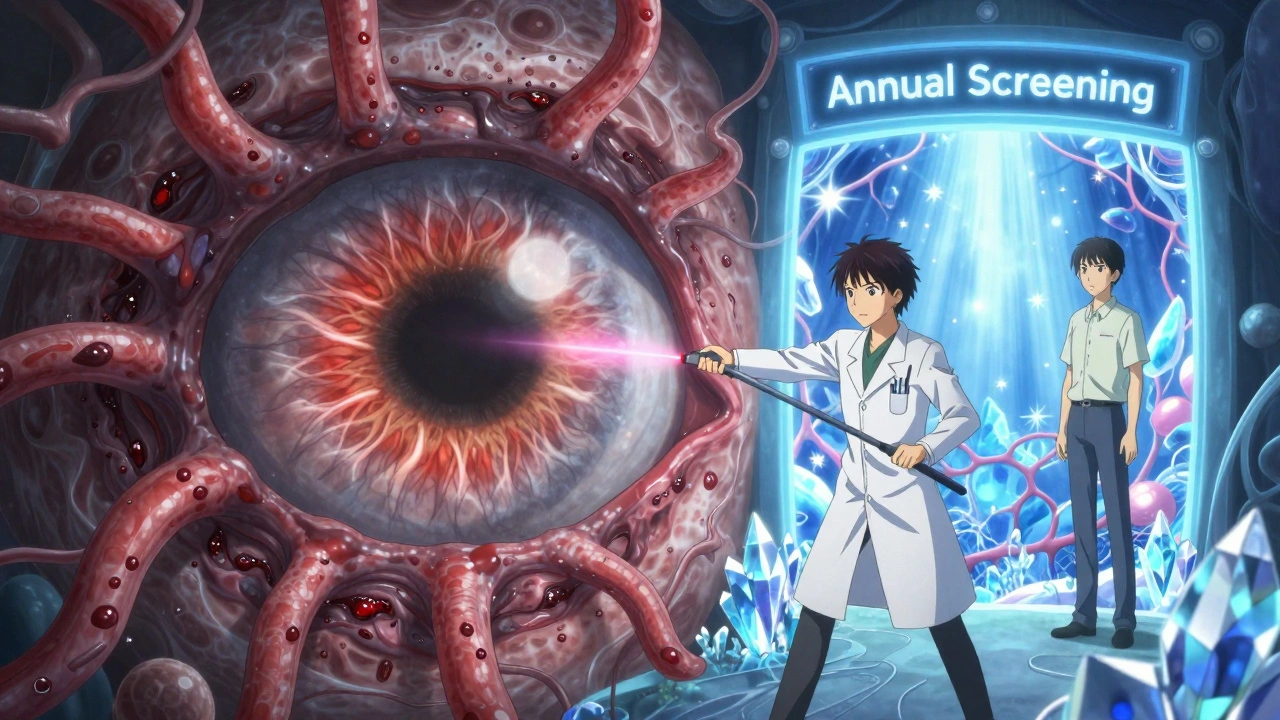
Diabetic Retinopathy: How High Blood Sugar Damages Your Eyes and What Laser Treatment Can Do

Every year, thousands of people with diabetes lose vision-not because of bad luck, but because they didn’t know their eyes were slowly being damaged. Diabetic retinopathy doesn’t come with warning signs. No pain. No sudden blur. Just quiet, creeping harm to the blood vessels in your retina. By the time you notice floaters, blurred vision, or dark spots, it’s often too late to fully reverse the damage. But here’s the truth: if you catch it early, you have a 95% chance of keeping your sight. And laser treatment isn’t just an option-it’s a lifeline for many.
What Exactly Is Diabetic Retinopathy?
Diabetic retinopathy is damage to the retina caused by high blood sugar over time. The retina is the light-sensitive layer at the back of your eye. It turns light into signals your brain reads as images. When blood sugar stays high for years, it starts chewing away at the tiny blood vessels that feed the retina. These vessels weaken, bulge, leak fluid, or even close off completely. In response, your eye tries to grow new blood vessels-but they’re fragile, messy, and useless. They bleed. They scar. They pull the retina away from its spot. That’s when vision starts to disappear.
This isn’t rare. About one in three adults with diabetes in the U.S. will develop some level of diabetic retinopathy. It’s the leading cause of vision loss in people aged 21 to 64. And here’s the scary part: most people don’t feel anything until it’s advanced. No symptoms at first. Just silent damage.
How Does It Progress?
Diabetic retinopathy doesn’t jump from zero to blind overnight. It moves in stages.
Mild nonproliferative stage: Tiny bulges called microaneurysms form in the retinal vessels. These are like weak spots in a garden hose. They might leak a little fluid, but you won’t notice. Your eye still sees clearly.
Moderate to severe nonproliferative stage: More vessels get blocked. The retina starts to swell, especially in the macula-the part responsible for sharp, central vision. This is called diabetic macular edema (DME). About 1 in 15 people with diabetes develop DME. Vision gets blurry, wavy, or distorted. Reading, driving, recognizing faces becomes hard.
Proliferative diabetic retinopathy: This is the danger zone. Because blood flow is cut off in parts of the retina, your eye tries to fix it by growing new blood vessels. But these vessels are like faulty wiring-they’re fragile, grow in the wrong places, and bleed easily. Blood can spill into the vitreous (the gel inside your eye), causing sudden floaters or even total vision blockage. Scar tissue forms and can pull the retina loose from the back of your eye. That’s a retinal detachment. It’s an emergency.
At this point, your vision might be gone-or close to it. That’s why waiting for symptoms is like waiting for your car to explode before checking the engine.
Why Laser Treatment Is Still a Game-Changer
When diabetic retinopathy reaches the proliferative stage-or when DME is threatening your central vision-laser treatment is often the first line of defense. It’s not glamorous. It’s not a cure. But it works.
The procedure, called panretinal photocoagulation, uses focused laser beams to seal leaking vessels and shrink abnormal ones. Think of it like welding broken pipes shut. The laser doesn’t restore lost vision. It stops further damage. In studies, it reduces the risk of severe vision loss by more than 50%.
For diabetic macular edema, doctors use a different kind of laser-focal laser therapy. This targets specific leaky spots near the macula. It doesn’t fix blurry vision overnight, but it stops it from getting worse. Many patients stabilize their vision after treatment. Some even regain a little clarity.
Laser treatment is quick. Usually done in an outpatient clinic. Local anesthetic drops numb your eye. You might feel a few bright flashes or mild discomfort. It’s not pleasant, but it’s over in minutes. Most people go home the same day.
It’s not magic. You’ll still need to manage your blood sugar. You’ll still need regular eye checks. But without laser therapy, the odds of losing vision skyrocket.

What Happens If You Don’t Treat It?
Ignoring diabetic retinopathy isn’t just risky-it’s reckless.
Without treatment, bleeding into the vitreous can cause sudden, dramatic vision loss. Scar tissue can pull the retina off the back of your eye. That’s a retinal detachment. It requires emergency surgery-and even then, vision may never fully return.
Another complication is neovascular glaucoma. New blood vessels grow over the drainage angle of your eye. Fluid can’t escape. Pressure builds. The optic nerve gets crushed. This form of glaucoma is extremely hard to treat and often leads to permanent blindness.
And once photoreceptor cells in your retina die from lack of oxygen? They’re gone forever. No medicine, no surgery, no miracle cure can bring them back. That’s why early detection isn’t just advice-it’s your only defense.
Who’s at Risk?
It’s not just how long you’ve had diabetes-it’s how well you’ve managed it.
- Duration of diabetes: If you’ve had diabetes for 10 years or more, your risk jumps dramatically.
- Poor blood sugar control: High HbA1c levels directly link to faster retinopathy progression. Keeping your average blood sugar below 7% cuts your risk significantly.
- High blood pressure: Every 10-point rise in systolic pressure increases your risk. Your eyes are sensitive to pressure changes.
- High cholesterol: Fatty deposits can clog retinal vessels, making damage worse.
- Pregnancy: Women with diabetes who get pregnant face a higher risk of rapid retinopathy progression. Regular eye checks during pregnancy are critical.
- Smoking: Smoking reduces oxygen in your blood and damages blood vessels. It’s like pouring gasoline on the fire.
Even if your diabetes feels "under control," retinopathy can still sneak up. That’s why screening isn’t optional.
Screening: Your Best Shield
Annual dilated eye exams are non-negotiable. That means drops to widen your pupils, so the doctor can see every corner of your retina. No vision test. No reading chart. Just a deep look at the blood vessels.
Some clinics now use digital retinal imaging-no dilation needed. A camera takes pictures of your retina while you stare into a light. It’s fast, painless, and surprisingly accurate. But it doesn’t replace a full exam by an ophthalmologist. If the images show anything suspicious, you still need to see the specialist.
Don’t wait for symptoms. Don’t skip your appointment because "your vision feels fine." That’s exactly when damage is happening.
People who get screened yearly and start treatment early have a 95% chance of preserving their vision. That’s not a guess. That’s what studies from UVA Health and the Cleveland Clinic show.
What Comes After Laser?
Laser treatment isn’t the end of the road. It’s a turning point.
Today, many patients get a combination of treatments. Anti-VEGF injections-medicines like ranibizumab or aflibercept-are now commonly used alongside or instead of laser for diabetic macular edema. These injections block the chemical that triggers abnormal blood vessel growth. They’re given as tiny shots into the eye, usually every few months.
Some patients need both laser and injections. Others need surgery if there’s heavy bleeding or retinal detachment. The goal isn’t one treatment. It’s long-term management.
And the foundation of all of it? Blood sugar control. No treatment works if your glucose levels stay high. Your eyes are a mirror of your overall diabetes health. If your HbA1c is 8.5%, no laser in the world will stop the damage.
What You Can Do Right Now
Here’s your action list:
- If you have diabetes and haven’t had a dilated eye exam in the last year-schedule one now.
- Check your HbA1c. If it’s above 7%, talk to your doctor about adjusting your plan.
- Control your blood pressure. Aim for under 130/80.
- Quit smoking. Even cutting down helps.
- Don’t ignore floaters, blurred vision, or dark spots. Call your eye doctor immediately.
Diabetic retinopathy doesn’t care how young you are, how active you are, or how "good" you think your diabetes is. It only cares about time and sugar. The good news? You’re not powerless. You have tools. You have options. You have time-if you act now.
What’s Next for Treatment?
Research is moving fast. Scientists are testing new drugs that target inflammation and nerve damage in the retina. Artificial intelligence is being trained to spot early signs of retinopathy in retinal scans-even before a doctor can. Telemedicine programs are now sending retinal images from rural clinics to specialists in cities, making screening accessible to more people.
But the core hasn’t changed: early detection + timely treatment + good diabetes control = preserved vision. That’s still the gold standard. And it’s still working.


I had no idea diabetic retinopathy could creep up like this. My uncle just lost vision in one eye last year and he swears he checked his sugar daily. Turns out, he never got his eyes checked. Lesson learned the hard way.
Early detection saves sight. This is not optional. It is medical necessity.
Wait so lasers are still a thing? I thought we had magic eye drops by now lol. Also my cousin got lasered and said it felt like someone was poking his eyeball with a hot nail. Not exactly comforting.
Just had my annual eye scan 😍 No dilation this time, just a quick snap with the camera. Felt like a spy movie. My doc said I'm clean! 🙌 Stay vigilant, fam!
For anyone reading this: if you have diabetes, get a dilated eye exam every year-even if your vision feels perfect. The damage is silent until it's not. Anti-VEGF injections and laser therapy aren't scary-they're shields. And HbA1c below 7%? That's your baseline, not a goal. Consistency beats perfection.
THIS. RIGHT HERE. I almost lost my job because I couldn't read the screen anymore. Turns out, I had diabetic macular edema. I thought it was just tired eyes. Laser treatment saved my career. I’m not exaggerating-this isn’t just about eyes. It’s about your life. Don’t wait. Don’t ignore. Go get checked.
So we're telling people to get lasers in their eyeballs because they didn't eat kale enough? Brilliant. Next we'll have mandatory eye vaccinations for eating toast. At least in Canada we just blame the sugar industry and go for maple syrup instead.
Many patients assume that if they don't have symptoms, they're fine. That's the most dangerous myth. Diabetic retinopathy progresses silently, and annual screening is the only reliable early warning system. Digital imaging helps, but it doesn't replace clinical evaluation. The combination of HbA1c control, blood pressure management, and timely intervention reduces vision loss risk by over 90%. This isn't opinion-it's evidence-based medicine.
My mom’s been diabetic for 22 years. She got her first laser treatment last year. Said it was weird but not unbearable. Now she checks her eyes every 6 months. She’s still driving, still reading, still baking pies. If she can do it, so can you. Just don’t wait until you can’t see the pie.
Laser treatment? That’s so 2010. Why aren’t we talking about gene therapy or stem cells? This post feels like it was written by a doctor who still uses fax machines. We’ve got AI that can detect retinopathy before the human eye. Stop glorifying outdated tech.
Man, I used to think diabetes was just about counting carbs. Turns out, it’s also about protecting your ability to see your kid’s first steps, your partner’s smile, your favorite sunset. This isn’t just medical advice-it’s a gift. Take it. Share it. Don’t let fear stop you from acting. You’ve got this.
Why are we even talking about lasers? The real problem is that American healthcare makes people wait months for screenings. If you’re poor, you don’t get checked until you’re blind. This post ignores the system. It’s not about willpower-it’s about access.