Dental Procedures on Blood Thinners: What You Need to Know About Bleeding Risk and Safety

Dental Procedure Risk Assessment Tool
Assess Your Dental Procedure Safety
This tool helps determine the safest approach for dental procedures while on blood thinners based on current medical guidelines.
Getting a tooth pulled or a deep cleaning while on blood thinners used to mean one thing: stop your meds. But that’s not the advice anymore. In fact, stopping your blood thinner for a simple dental visit could be riskier than keeping it. The real question isn’t whether you can get your teeth worked on - it’s how to do it safely without putting yourself in danger of a clot or a bleed.
Why Blood Thinners Are So Common Now
More people than ever are on blood thinners. It’s not just older adults with atrial fibrillation anymore. A 28-year-old athlete might be on one after a blood clot from a long flight. A new mom could be taking it after a pulmonary embolism. Even someone young and healthy might need it after surgery or due to a genetic condition like factor V Leiden. Today, about 60% of new prescriptions are for direct oral anticoagulants (DOACs) like apixaban, rivaroxaban, or dabigatran. Warfarin is still around, but it’s no longer the go-to.These drugs prevent strokes, heart attacks, and dangerous clots in the legs or lungs. Stopping them - even for a few days - can trigger a clot that’s far more dangerous than any bleeding from a tooth extraction. Studies show that holding these medications for minor dental work doesn’t reduce bleeding much, but it sharply increases the chance of a life-threatening clot.
Not All Dental Procedures Are the Same
You don’t need to panic if you’re on blood thinners. Most dental work is low-risk and completely safe to do without changing your meds. Here’s how procedures break down:- Low-risk: Routine checkups, X-rays, cleanings, fillings, crowns, root canals. No need to stop your blood thinner. Ever.
- Low-moderate risk: Deep cleaning (scaling and root planing), single tooth extractions. Again, most guidelines say: keep taking your meds. No hold needed.
- Moderate risk: Removing 2-3 teeth, gum surgery, bone removal, complex extractions. Here’s where things get a little more careful - but still, stopping your blood thinner isn’t automatic.
Stanford Health Care and the Scottish Dental Clinical Effectiveness Programme (SDCEP) both agree: for low and low-moderate risk procedures, continuing your anticoagulant is the safest choice. The American Dental Association’s 2022 update says the same thing. The old rule - stop everything before dental work - is outdated and dangerous.
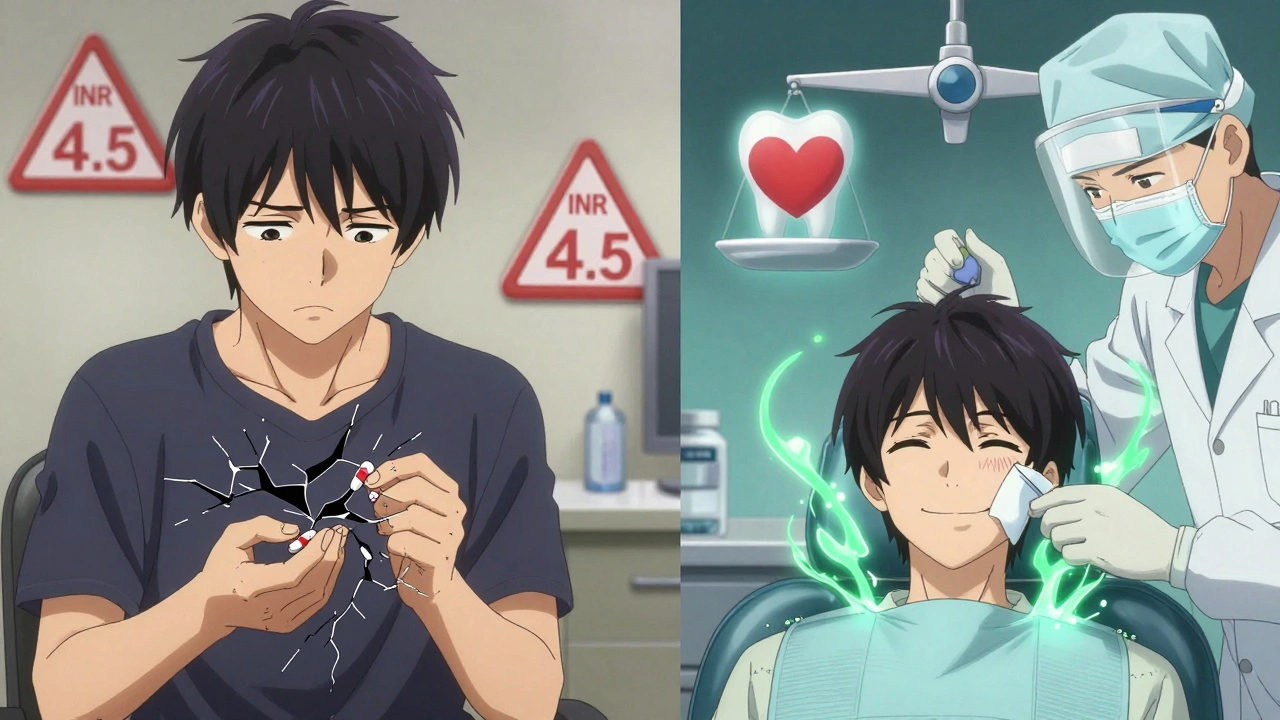
What About Your INR Level?
If you’re on warfarin, your doctor checks your INR (International Normalized Ratio) to see how thin your blood is. This number matters - but not as much as you might think.- For low-risk procedures: INR under 3.5 is fine. Most people on warfarin are already in this range.
- For low-moderate risk: INR under 3 is ideal. If you’re over 3, talk to your doctor - but don’t assume you need to stop.
- For moderate procedures: INR under 3.5 is acceptable if your dentist uses extra hemostatic techniques.
Here’s the catch: if your INR is above 4.0, your risk of bleeding goes up. But even then, stopping warfarin isn’t always the answer. Your doctor might adjust your dose instead of stopping it completely. The goal is to keep your INR in the therapeutic range - not to drop it to normal.
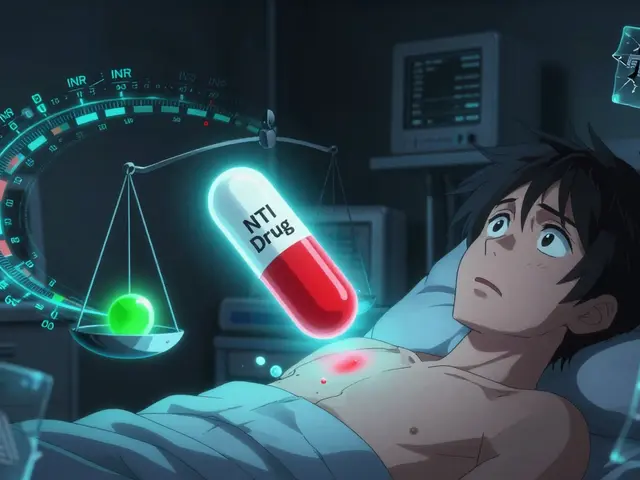
DOACs: The New Normal
If you’re on a DOAC like Eliquis or Xarelto, the rules are simpler - and more straightforward.- For most procedures: No need to skip a dose. Keep taking it.
- For moderate-risk extractions: Some guidelines suggest skipping the morning dose on the day of surgery. That’s it. No multi-day hold.
- Timing matters: If you do skip a dose, schedule your procedure at least 4 hours after your last pill. That’s when drug levels are lowest.
DOACs leave your system faster than warfarin. That’s why you don’t need to stop them days in advance. Stopping early doesn’t help much - and it raises your clot risk. The CHEST 2022 guidelines say skipping just one dose is enough for most cases.
What Your Dentist Should Do to Control Bleeding
Even if you’re on blood thinners, bleeding after a tooth extraction is usually minor and easy to stop. Dentists have tools for this.- Tranexamic acid mouthwash: A 5% solution held in the mouth for 1-2 minutes, repeated every 2 hours for the first day. It’s not magic, but it works. One study showed it cuts bleeding time in half.
- Pressure: Gauze packed tightly over the extraction site for 30-60 minutes. Bite down firmly. Don’t spit or rinse for 24 hours.
- Sutures: If needed, stitches help close the wound and reduce bleeding.
- Avoid multiple extractions: Don’t pull three teeth in a row. Space them out. One or two at a time is safer.
And here’s something you might not know: avoid NSAIDs like ibuprofen or naproxen after surgery. These drugs thin your blood too. Use acetaminophen (Tylenol) instead for pain. Also, watch out for antibiotics like clarithromycin or antifungals like fluconazole - they can interact with DOACs and raise bleeding risk.
When You Should Stop Your Blood Thinner
There are only a few cases where stopping makes sense:- Multiple complex extractions (4+ teeth)
- Major oral surgery (jaw reconstruction, tumor removal)
- Patients with a history of severe bleeding on anticoagulants
- INR above 4.5 with no clear reason
Even then, it’s not a blanket stop. Your doctor and dentist need to talk. They might bridge you with heparin injections instead of stopping everything. Or they might just delay the procedure a few days while adjusting your dose.
Don’t ever stop your blood thinner on your own. Not even for a day. I’ve seen patients stop warfarin because their dentist told them to - and end up in the ER with a stroke three days later.

What You Should Do Before Your Appointment
Here’s your checklist:- Bring a list of every medication you take - including supplements. Some herbs like ginkgo, garlic, or fish oil can also thin your blood.
- Know your current INR (if on warfarin) or your last DOAC dose time.
- Tell your dentist exactly why you’re on blood thinners. It’s not just a formality - it changes their plan.
- Ask: "Do you have tranexamic acid mouthwash on hand?" If they say no, they might not be up to date on current guidelines.
- Don’t take aspirin or NSAIDs before your appointment. Stick to acetaminophen if you need pain relief.
What to Do After Your Procedure
Follow your dentist’s instructions. But here’s what to watch for:- Light pink saliva for the first 24 hours? Normal.
- Bright red bleeding that won’t stop after 2 hours of pressure? Call your dentist.
- Swelling, fever, or foul taste? Could be infection - not bleeding.
- Shortness of breath, chest pain, or sudden weakness? Go to the ER. That’s a clot - not a dental issue.
Most bleeding stops with gauze and time. But if you’re worried, call your dentist. Better safe than sorry.
Bottom Line: Keep Taking Your Blood Thinners
The biggest mistake people make is thinking blood thinners = danger at the dentist. The truth? The danger is in stopping them.For 9 out of 10 dental procedures, you don’t need to change a thing. Your dentist can handle the bleeding. Your doctor can help if your INR is too high. And you? You just need to speak up, show up prepared, and trust the updated guidelines.
Modern dentistry doesn’t ask you to choose between a healthy mouth and a healthy heart. It gives you both - if you know how to ask for it.
Can I still get a tooth pulled if I’m on blood thinners?
Yes, absolutely. Most single tooth extractions are safe to perform while you’re on blood thinners. The key is not stopping your medication - it’s using proper hemostatic techniques like tranexamic acid mouthwash and pressure. Your dentist should be familiar with current guidelines from the ADA and SDCEP. Stopping your blood thinner for a simple extraction increases your risk of stroke or clot far more than it reduces bleeding.
Should I stop warfarin before a dental cleaning?
No. Routine cleanings, X-rays, and exams are low-risk procedures. Stopping warfarin for these is unnecessary and dangerous. Your INR should be checked regularly anyway - if it’s under 3.5, you’re fine to proceed. The American Dental Association confirms that altering anticoagulation for routine dental care offers no benefit and increases clot risk.
Do DOACs like Eliquis or Xarelto need to be stopped for dental work?
For most dental procedures, no. You can keep taking them. For moderate-risk procedures like multiple extractions, skipping the morning dose on the day of surgery is sometimes recommended. But don’t stop for days. DOACs clear from your system in 12-24 hours, so a single missed dose is enough to reduce bleeding risk without increasing clot danger. Always check with your doctor before making any changes.
What if my INR is too high? Should I delay my dental appointment?
If your INR is above 4.5, your dentist may recommend postponing non-emergency procedures until your levels are better controlled. But don’t panic - this doesn’t mean you can’t get care. Your doctor can adjust your warfarin dose, and your dentist can still treat you safely with extra hemostatic measures. Never try to lower your INR by skipping doses yourself - that’s how clots happen.
Can I take ibuprofen or aspirin after a tooth extraction if I’m on blood thinners?
No. Avoid NSAIDs like ibuprofen, naproxen, and aspirin entirely. These drugs also thin your blood and can increase bleeding risk when combined with anticoagulants. Use acetaminophen (Tylenol) for pain instead. If your dentist prescribes a painkiller, ask if it interacts with your blood thinner. Many antibiotics and antifungals can too - so always give your full medication list to your dentist.


i was so scared to get my wisdom teeth out on Eliquis but my dentist was like 'nah, just skip your morning dose' and i did and it was fine. no bleeding like a horror movie. honestly, most dentists are way behind on this stuff.
So now we’re supposed to trust dentists with our lives because some 'guidelines' say so? What’s next? Letting barbers do open-heart surgery because 'it’s low risk'? This is how people die. You think your INR is safe? Maybe you’re just lucky.
OMG YES. My dentist had tranexamic acid and i was like 'wait you actually know what this is?' and she said 'of course, we’ve been doing this for years.' Why do so many docs still tell people to stop their meds? It’s insane. I almost had a stroke once because my old dentist made me stop warfarin for a cleaning. Don’t let that happen to you.
The underlying assumption here-that bleeding is a manageable variable while thrombosis is an existential threat-is philosophically profound. We’ve inverted the medical hierarchy: where once we feared hemorrhage as the ultimate failure, now we recognize that the body’s clotting cascade, when dysregulated, is the silent architect of mortality. The real tragedy isn’t the post-op ooze-it’s the systemic ignorance that still equates anticoagulation with vulnerability rather than resilience.
They say 'don't stop your meds' but who really controls the system? Pharma companies wrote these guidelines. They profit from DOACs. They don’t care if you bleed a little. They care if you keep buying pills. Wake up.
YES!! I just had a cleaning last week and my dentist gave me the tranexamic acid rinse. I felt so cared for 😭 thank you for sharing this!! Everyone should read this!!
Modern dentistry has become a ritual of compliance with corporate protocols masquerading as clinical wisdom. The notion that a single missed dose of rivaroxaban is sufficient to mitigate bleeding risk is a statistical fiction engineered to reduce liability not to preserve life. Your dentist is not your guardian. Your doctor is not your oracle. You are the only one who understands the calculus of your own mortality and the cost of convenience.
They’re lying to you. The CDC knows that blood thinners are used to control populations. Dentists are just the front line. If you stop your meds, you’re safe. If you don’t, you’re a lab rat. They want you bleeding so they can sell you more drugs. Look up Operation Blue Shield. It’s all connected.
My dad had a tooth pulled on Xarelto and they just used gauze and told him not to rinse. He’s fine. Just listen to your dentist and don’t panic. It’s not that complicated.
Let’s quantify this. The 2022 ADA meta-analysis showed a 0.03% absolute increase in bleeding with continued anticoagulation versus a 1.8% absolute increase in thromboembolic events with interruption. The risk-benefit ratio is mathematically indefensible if you’re not continuing. Anyone who says otherwise is either misinformed or has a conflict of interest. Period.
My cousin in Delhi had a root canal on apixaban. Dentist used local anesthesia with epinephrine and packed the socket with gauze soaked in tranexamic acid. No issues. It’s not magic, it’s just standard now. The real issue is access-many clinics here still don’t have the rinse. Education matters more than guidelines.
Wow. So now we’re supposed to trust a dentist who probably didn’t even pass biochemistry to make decisions about my anticoagulation? I mean, come on. I’ve read the guidelines. I’ve read the CHEST papers. I’ve read the Cochrane reviews. And I still don’t trust it. My dentist says 'just skip the morning dose' like it’s a coffee order. I’m going to my hematologist tomorrow. This is too risky.
Let us not forget the historical context of this paradigm shift. For decades, the medical establishment operated under the assumption that bleeding was the primary adversary in anticoagulated patients. This was a relic of an era when hemostatic agents were primitive, when INR monitoring was crude, and when DOACs were not yet conceived. The transition to current protocols represents not merely a clinical evolution but a philosophical rebirth-a recognition that the body’s innate clotting mechanisms, when left undisturbed, are more than capable of sealing a minor wound. To interrupt this delicate equilibrium for the sake of perceived safety is not caution-it is hubris. And yet, we still cling to the ghost of outdated dogma, whispering 'stop your meds' like a prayer in a cathedral of ignorance. The truth is not in the guidelines. The truth is in the silence between the heartbeat and the clot.