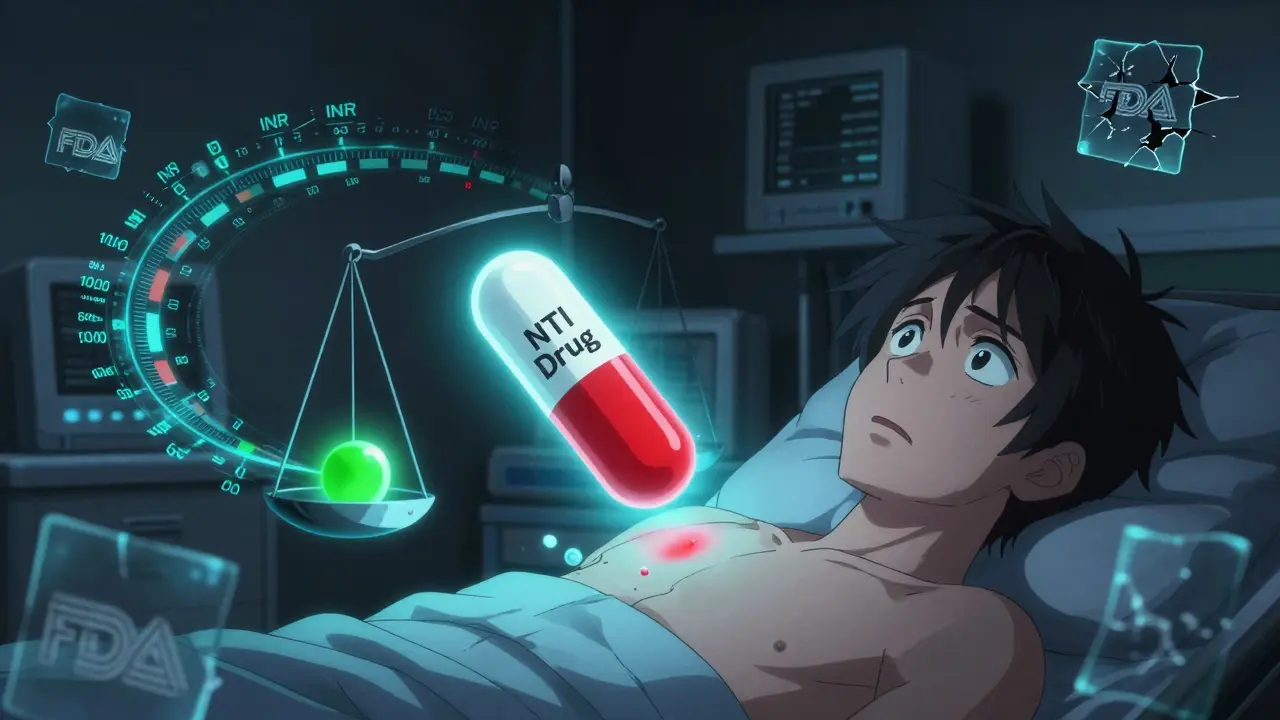
Studies show that switching to generic versions of NTI drugs like warfarin, phenytoin, and cyclosporine can lead to unstable blood levels, increased side effects, and serious health risks-even when generics are FDA-approved. What the data reveals about real-world outcomes.
Warfarin: What It Is, How It Works, and What You Need to Know
When you take warfarin, a prescription blood thinner used to prevent dangerous clots in the heart, legs, or lungs. Also known as Coumadin, it's one of the most commonly prescribed anticoagulants in the world. But unlike most meds, warfarin doesn’t just work and you’re done. It’s a tightrope walk between preventing clots and causing dangerous bleeding. One day you’re fine, the next, a small cut takes forever to stop. That’s because warfarin’s effect changes based on what you eat, what else you take, and even your genetics.
Warfarin works by blocking vitamin K, which your body needs to make clotting factors. That’s why foods rich in vitamin K — like spinach, kale, broccoli, and Brussels sprouts — can make it less effective. But you don’t need to quit greens cold turkey. Consistency matters more than avoidance. Eat the same amount every week, and your doctor can adjust your dose accordingly. The real danger comes from mixing warfarin with other drugs. Antibiotics, antifungals, even some OTC pain relievers like ibuprofen can spike your INR, the test that measures how long your blood takes to clot. A high INR means you’re at risk of bleeding. A low one means you’re not protected enough from clots. That’s why regular blood tests aren’t optional — they’re life-saving.
People on warfarin often don’t realize how many things can throw off their balance. Stopping or starting an herbal supplement like garlic, ginkgo, or even St. John’s wort? That’s a red flag. Even switching brands of warfarin — even if they’re both generics — can cause problems because the absorption isn’t always identical. That’s why your doctor might stick with the same brand for years. And if you’re on warfarin and suddenly need surgery, dental work, or even a colonoscopy, you can’t just skip your pill. You need a plan. Some people switch to heparin injections temporarily. Others pause warfarin and restart after. It’s not guesswork — it’s protocol.
There’s no sugarcoating it: warfarin demands attention. But for millions of people with atrial fibrillation, artificial heart valves, or a history of deep vein thrombosis, it’s the best tool they’ve got. Newer blood thinners like apixaban or rivaroxaban don’t need constant testing, but they’re not always cheaper, covered by insurance, or right for every body. Warfarin is old, it’s cheap, and if you manage it right, it works. The key isn’t fear — it’s awareness. Know your numbers. Know your diet. Know what you’re taking alongside it. And never, ever skip a checkup.
Below, you’ll find real-world advice on managing warfarin safely — from spotting hidden interactions to understanding why your INR jumped last week. These aren’t theory pieces. They’re lessons from people who’ve been there.
Most dental procedures are safe while on blood thinners. Learn when to keep taking your meds, how dentists control bleeding, and what to avoid - based on 2025 guidelines.