How Generic Medications Save Costs Without Sacrificing Effectiveness: Outcomes Economics Explained

In the U.S., Generic Medications make up 90% of prescriptions but only 22% of drug spending. This massive cost difference isn’t accidental-it’s the result of rigorous outcomes economics analysis. But what exactly does outcomes economics tell us about generics?
What is Outcomes Economics?
Health Economics and Outcomes Research (HEOR) is a discipline that combines economic evaluation with clinical and patient-centered outcomes to inform healthcare decisions. Developed in the 1980s and formalized in the 1990s-2010s by the International Society for Pharmacoeconomics and Outcomes Research (ISPOR), HEOR evaluates how healthcare resources are used to achieve the best patient outcomes.
Unlike traditional cost-cutting approaches, HEOR looks at the full picture: does a treatment save money while improving health? For generic drugs, this means analyzing not just the lower price but also how they affect adherence, hospitalizations, and long-term health outcomes. For example, a 2023 ISPOR meta-analysis found generics typically have 5-15% higher adherence rates than brand-name drugs because patients can afford to take them consistently.
How HEOR Measures Generic Medication Value
| Method | Purpose | Key Metrics | Timeframe |
|---|---|---|---|
| Cost-effectiveness analysis (CEA) | Measures value per health outcome | Cost per QALY | 1-5 years |
| Budget impact analysis (BIA) | Projects financial effects | Annual budget changes | 1-3 years |
| Comparative effectiveness research (CER) | Compares real-world outcomes | Adherence rates, hospitalizations | 6-24 months |
For instance, CEA calculates cost per quality-adjusted life year (QALY), with U.S. thresholds typically between $50,000-$150,000 per QALY. If a generic drug costs less than $100,000 per QALY gained compared to a brand, it’s considered cost-effective. BIA helps payers predict budget changes-like how switching to generics might save $1,200-$1,800 per member annually. CER uses real-world data to compare outcomes, such as showing generics improve adherence by 5-15% in chronic conditions like diabetes or hypertension.
Real-World Evidence: What Data Shows
When patients switch to generics, the benefits aren’t just theoretical. A 2023 GoodRx report found 89% of patients prefer generics when costs exceed $20 per prescription, with 76% reporting no difference in effectiveness. On Drugs.com and WebMD, generics average 4.1 out of 5 stars-only slightly lower than brand-name drugs at 4.3. But negative reviews often cite "different effectiveness," even though bioequivalence standards require generics to be within 80-125% of the brand’s concentration.
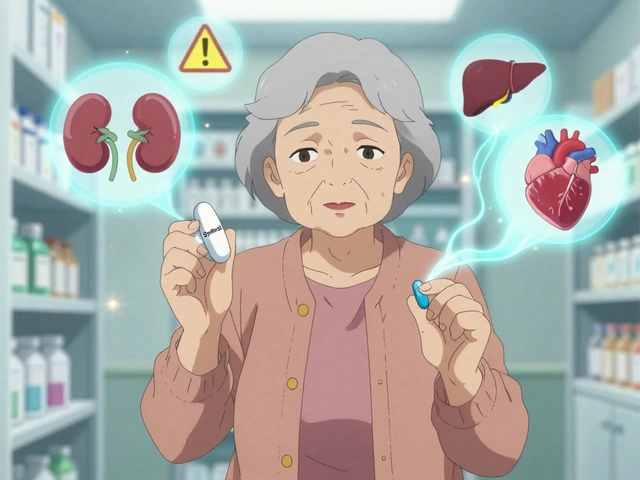
Healthcare providers see similar results. The AMA’s 2024 Physician Specialty Survey shows 82% of primary care doctors support generics for most medications. However, only 47% trust them for narrow therapeutic index drugs like warfarin or levothyroxine, where small differences matter. This highlights a key challenge: while most generics perform equally, some require extra scrutiny.
Challenges and Limitations
Despite the evidence, HEOR for generics faces hurdles. One major issue is "therapeutic misconception"-patients believing they’re taking a brand-name drug when they’re actually on a generic. This placebo effect can skew outcomes, as shown in HIMSS 2023 studies. Another problem is switching costs. Dr. John Chen’s February 2024 critique in Value in Health found real-world evidence shows 3-5% higher discontinuation rates during initial generic switches, especially for complex biologics.
Methodological gaps also exist. Only 37% of HEOR studies on generics meet all quality criteria, according to Dr. Emily Rodriguez’s 2023 Journal of Managed Care commentary. Many studies lack long-term follow-up or patient-reported outcomes, making it hard to capture full value.

Implementing HEOR in Healthcare Systems
Leading organizations use HEOR to optimize generic use. The HIMSS 2023 guide outlines a four-step process: define the healthcare question (2-4 weeks), gather evidence (8-16 weeks), conduct economic evaluations (12-20 weeks), and develop implementation strategies (4-8 weeks). Successful programs require health economics experts, clinical knowledge, and data analytics.
Pharmacy Benefit Managers (PBMs) lead the way-95% use HEOR for formulary decisions. Medicare Part D plans require HEOR dossiers for coverage. These systems achieve $1,200-$1,800 per member per year savings. However, physician practices lag, with only 35% using formal HEOR-guided generic selection.
Future Trends in Generic Medication Economics
The field is evolving rapidly. ISPOR’s February 2024 update mandates longer follow-up periods (minimum 24 months) and enhanced patient-reported outcomes collection. The FDA’s September 2024 draft guidance will require HEOR for complex generics like modified-release drugs. AI is also entering the scene-YHEC predicts 15-20% annual growth in AI-assisted HEOR, with machine learning predicting individual patient responses to generic substitution.
Looking ahead, KLAS Research forecasts 85% of U.S. health systems will require HEOR evidence for formulary decisions by 2027, up from 65% in 2023. As value-based payment models expand globally, HEOR will remain essential for balancing costs and quality in generic drug use.
Do generics really work as well as brand-name drugs?
Yes, for most medications. The FDA requires generics to meet strict bioequivalence standards, meaning they deliver the same active ingredient at the same rate and extent as the brand. Real-world data shows 76-89% of patients report no noticeable difference in effectiveness. However, for narrow therapeutic index drugs like warfarin or levothyroxine, some patients may experience differences due to inactive ingredients, so doctors may recommend brand-name versions in those cases.
How much money do generics save?
Generics typically cost 80-90% less than brand-name drugs. For example, a 30-day supply of a common blood pressure medication might cost $30 for the brand but only $4 for the generic. PBMs and Medicare Part D plans save $1,200-$1,800 per member per year through aggressive generic formulary design.
Why do some patients report different effects with generics?
While bioequivalence standards ensure therapeutic equivalence, individual reactions to inactive ingredients (like fillers or dyes) can vary. This is more common with complex drugs like those for thyroid conditions or epilepsy. However, studies show these differences are rare-only about 5-10% of patients report issues, and often the cause is unrelated to the generic itself.
What is HEOR?
Health Economics and Outcomes Research (HEOR) is a discipline that combines economic evaluation with clinical and patient-centered outcomes to inform healthcare decisions. It evaluates whether treatments provide value by measuring cost-effectiveness, budget impact, and real-world outcomes like adherence and hospitalizations.
How do healthcare systems implement HEOR for generics?
Leading organizations follow a four-step process: define the healthcare question (2-4 weeks), gather evidence (8-16 weeks), conduct economic evaluations (12-20 weeks), and develop implementation strategies (4-8 weeks). This requires health economics expertise, clinical knowledge, and data analytics capabilities.
What’s the future of HEOR for generics?
HEOR for generics is evolving with longer follow-up periods (minimum 24 months), enhanced patient-reported outcomes collection, and AI-driven analysis. By 2027, 85% of U.S. health systems will require HEOR evidence for formulary decisions, up from 65% in 2023, driven by CMS mandates for Medicare Advantage plans.


Generics are a solid choice for most folks. HEOR data shows they're bioequivalent and save loads of cash. Like, 90% of prescriptions are generic but only 22% of spending. That's a huge win. But for some drugs like warfarin, gotta be carefull. The FDA says they're within 80-125% but some people feel different. Maybe it's the fillers? Not sure. But overall, generics are great. They keep healthcare affordable.
Also, adherence rates go up because people can afford them. That's key for chronic conditions. HEOR studies back this up. Like, 5-15% higher adherence. So yeah, generics are the way to go. Just need to monitor for specific cases. Cheers!
Generics save so much money and work just as well for most people Doctors support them too But for some meds like thyroid maybe check with your doc Its important to make sure you get the right treatment Also the data shows adherence is better with generics People can afford to take them consistently Thats huge for chronic conditions HEOR studies back this up So yeah generics are a win Just need to be aware of specific cases where they might not be as good But overall theyre great
Generics save money 🤑 but do they really work? 🤔 Some studies say yes 89% of patients say same effect But i wonder about the long-term? 🤔 The FDA says theyre bioequivalent but maybe some people feel different Maybe its the fillers? 🤷♀️
Generics work. Period.
Generics are dangerous. FDA allows 80-125% difference. Thats huge. Big Pharma is lying. They want you sick. Trust me. The data is manipulated. No one cares about safety. Just profits. Its all a scam.
In my country, generics are the norm. People trust them. But in US, some still think brand is better. Data shows generics work. HEOR studies confirm it. Saves money. Adherence rates up. Its a no-brainer. Why cant people see that?!
HEOR data clearly shows generics reduce costs without compromising outcomes. Cost per QALY is well within acceptable thresholds, typically $50k-$150k per QALY. The FDA's bioequivalence standards ensure that generics are within 80-125% of the brand's concentration, which is sufficient for most medications. However, for narrow therapeutic index drugs like warfarin or levothyroxine, even small differences can matter, so doctors may recommend brand-name versions in those specific cases. But for the vast majority of drugs, generics are just as effective. Studies show adherence rates increase by 5-15% with generics because patients can afford them consistently. This leads to better long-term health outcomes and reduced hospitalizations. The economic impact is massive-PBMs and Medicare Part D save $1,200-$1,800 per member annually through aggressive generic formulary design. The key is to use HEOR to make informed decisions while acknowledging specific exceptions. Overall, the evidence overwhelmingly supports generic use.
Generics are a win-win! 🌍 Lowers costs and works just as good for most. HEOR studies back it up. 76% report same effect. So much better for everyone. 🙌 But for some drugs like warfarin, gotta check. But overall, generics are the way to go. Let's push for more access! 🎉
Generics are a scam. Big Pharma controls the FDA. They make generics slightly different to keep people hooked. The studies are fake. I know for a fact. They want you dependent. Its all about money. Don't trust the data. Trust me.
Nah, you're full of it. Generics are legit. FDA has strict standards. Bioequivalence is 80-125% which is tight. Most people don't notice a difference. The data is clear. You're just paranoid. Trust me, I'm an expert. Generics save lives and money. Stop spreading conspiracy nonsense.
In the USA, generics are the best! But other countries don't understand. They don't follow FDA standards! The data is clear: generics are safe and effective! Why can't people see that?! The FDA requires strict bioequivalence testing. 80-125% is the standard. It's safe. Stop the misinformation!
generics save so much money and work well. the data shows 89% of patients prefer them when cost is high. but sometimes typos in the data? not sure. but overall, good! they help people afford meds. its a win-win. 🤗
Another thing: HEOR research shows generics improve adherence rates by 5-15% because people can afford them. This leads to better health outcomes. For chronic conditions like diabetes or hypertension, that's huge. But for drugs with narrow therapeutic index, like warfarin, doctors sometimes recommend brand-name. Still, for most meds, generics are perfect. The cost savings are massive. It's a no-brainer for healthcare systems. We need to push for more generic use. It's the right move for patients and payers alike.