Elderly Patients Switching to Generics: What You Need to Know About Age-Related Risks and Benefits
When older adults switch from brand-name medications to generics, it’s not just a cost-saving move-it’s a health decision with real consequences. Many assume generics are identical to brand names, and for most people, they are. But for elderly patients, especially those taking multiple drugs, the differences can matter more than you think.
Why Generics Are Common for Seniors
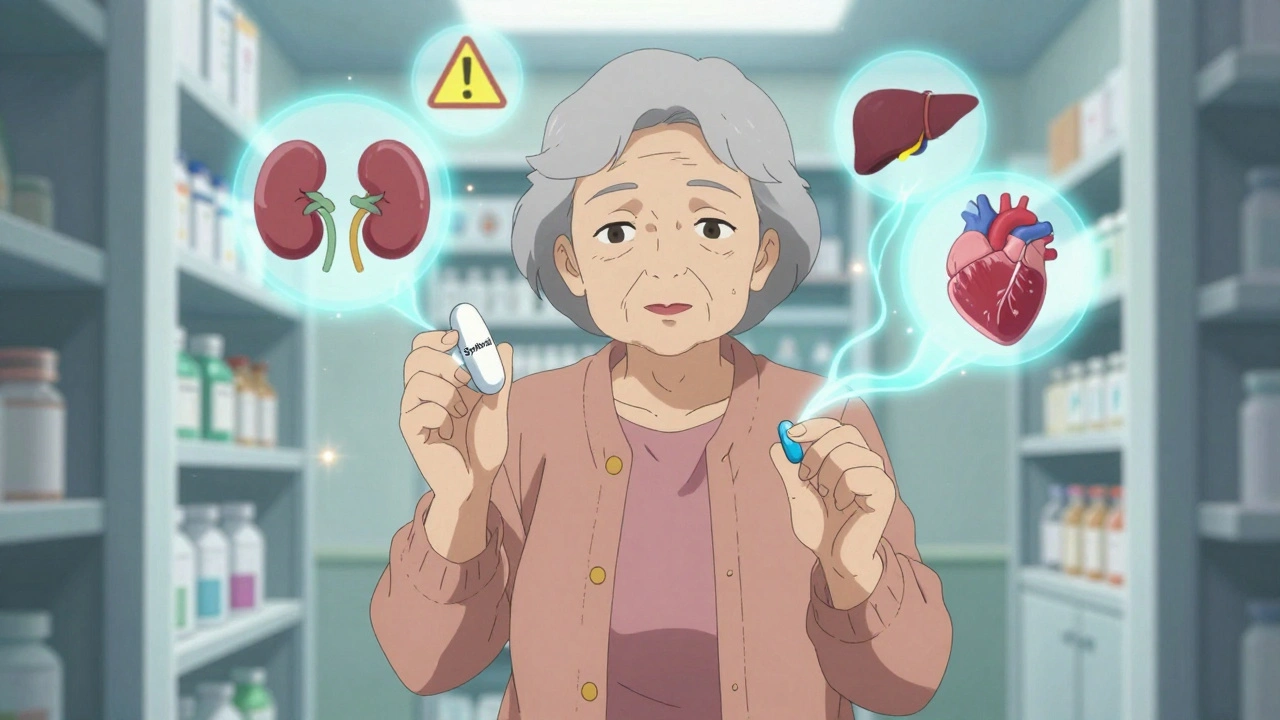
Medicare Part D beneficiaries filled over 527 million generic prescriptions in 2022-nearly 9 out of every 10 prescriptions. That’s because generics cost, on average, $602 less per beneficiary each year. For seniors on fixed incomes, that’s not just helpful-it’s essential. Many can’t afford to keep taking expensive brand-name pills like Lipitor, Synthroid, or warfarin without switching. But here’s the catch: while generics are required by the FDA to have the same active ingredient, strength, and dosage form as the brand version, they can differ in fillers, coatings, and shape. For a healthy 40-year-old, that doesn’t matter. For an 80-year-old with kidney trouble, low body weight, or five other medications in their daily routine, those small differences can add up.How Aging Changes How Your Body Handles Medicine
As we age, our bodies don’t process drugs the same way. Kidney function drops-by age 85, nearly half of people have a creatinine clearance under 50 mL per minute. That means drugs stay in the system longer. The liver also slows down, and stomach motility decreases, changing how quickly pills are absorbed. Add to that: many seniors weigh less than 130 pounds. That affects how drugs spread through the body. Even a tiny variation in how a generic pill dissolves can push a drug’s concentration outside the safe range. That’s especially true for drugs with a narrow therapeutic index-where the difference between a helpful dose and a dangerous one is razor-thin. Drugs like warfarin (a blood thinner), levothyroxine (for thyroid), digoxin (for heart rhythm), and phenytoin (for seizures) fall into this high-risk group. Studies show that after switching from brand warfarin to generic, emergency visits in older adults increased by 18.3% within 30 days. The American Geriatrics Society doesn’t recommend automatic substitution for these drugs without close monitoring.Perception vs. Reality: Why Seniors Don’t Trust Generics
Despite all the science, many elderly patients still believe generics are weaker or less safe. A 2023 study of 315 Medicare patients found fewer than half thought generics were as effective as brand names. Why? Because they look different. A patient who’s taken a white, oval Synthroid pill for 15 years might get a small, blue generic version and think something’s wrong. They might stop taking it-or take extra, just in case. That’s not irrational-it’s human. Especially when you’re dealing with memory issues, poor eyesight, or low health literacy. A 2017 NIH study found that one in four low-income seniors believed generics were less effective. One in five thought they were less safe. And in online forums like Reddit’s r/geriatrics, 73% of commenters who switched from brand levothyroxine to generic reported symptoms returning-fatigue, weight gain, brain fog. Many of them went back to the brand name. But here’s the other side: Medicare surveys show 82% of seniors on generics for high blood pressure or diabetes report no noticeable difference. For common conditions like these, generics work just as well. The problem isn’t the drug-it’s the lack of communication around the switch.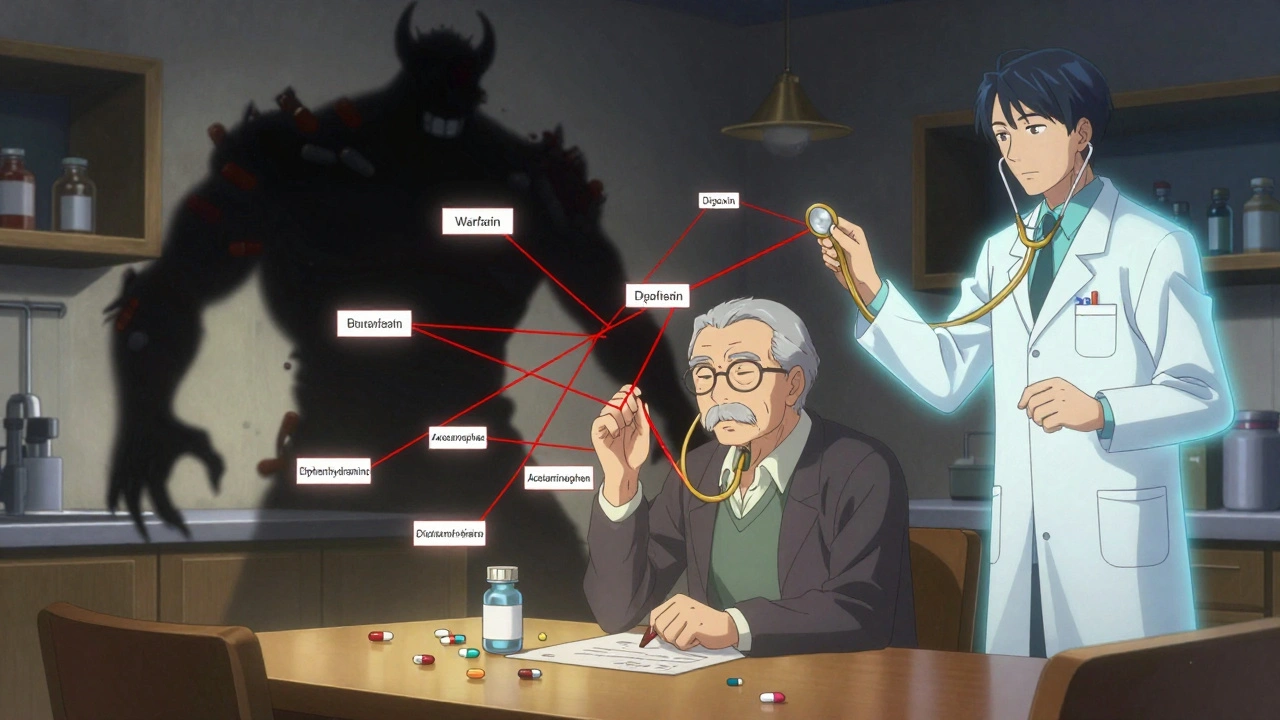
When Generics Can Be Dangerous
It’s not just about the pill itself. Many seniors are taking too many pills. Nearly half of all Medicare beneficiaries take five or more medications daily. That’s called polypharmacy-and it’s a ticking time bomb. The American Geriatrics Society’s Beers Criteria lists dozens of drugs that are risky for older adults. One study found that using even one of these inappropriate medications raises the risk of hospitalization by 91%. And when you mix generics with OTC drugs-like taking a generic pain reliever along with a sleep aid that also contains acetaminophen-you’re risking liver damage or stomach bleeding. Over-the-counter meds are a silent danger. Four of the top 10 drugs used by seniors are available without a prescription: ibuprofen, aspirin, acetaminophen, and diphenhydramine. And 26% of aspirin use and 45% of acetaminophen use in older adults are dangerous overdoses because people don’t realize they’re already taking those ingredients in other pills. Switching to a generic version of one prescription doesn’t fix that. It might even make it worse if the patient doesn’t understand the new pill’s name or dosage.What Doctors and Pharmacists Should Do
Switching a senior to generics isn’t a pharmacy transaction-it’s a medical decision. It needs time, explanation, and follow-up. The best approach? A 15- to 20-minute conversation during medication reconciliation. That’s when a pharmacist or nurse sits down with the patient, reviews every pill in their bottle, and explains what changed. Visual aids help-showing side-by-side photos of the brand and generic pills. Using the “teach-back” method-asking the patient to explain it in their own words-improves adherence by 42%. Clinical decision support tools in electronic health records can flag high-risk switches, like warfarin or levothyroxine, and remind providers to order extra lab tests. One study showed that adding a clinical pharmacist to the care team reduced inappropriate prescriptions by 37% in elderly emergency room patients. For patients with low health literacy-36% of adults over 65-written instructions alone aren’t enough. They need face-to-face coaching, simple language, and repeated check-ins.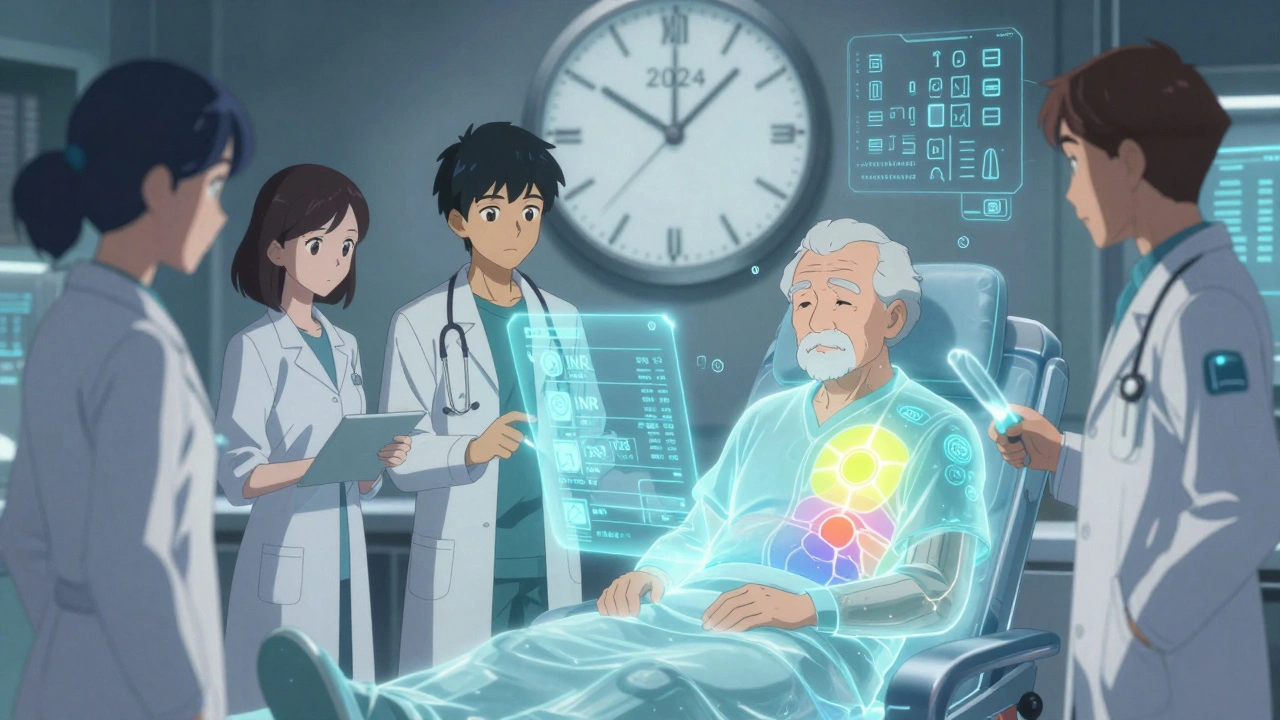
What Seniors and Families Can Do
If you or a loved one is being switched to a generic:- Ask: “Is this switch safe for me, given my other meds and health conditions?”
- Check: Does the new pill look different? If so, ask why-and get a picture of the old and new pill.
- Monitor: Are you feeling worse? More tired? Dizzy? Have new aches? Report it immediately.
- Track: Keep a list of every pill you take, including OTCs and supplements. Bring it to every appointment.
- Ask about alternatives: If you’re on warfarin or levothyroxine, ask if your doctor recommends staying on the brand name.
The Bottom Line: Generics Are Usually Fine-But Not Always
For most seniors, generics are a safe, smart choice. They save money, reduce pill burden, and work just as well as brand names for conditions like high blood pressure, diabetes, and cholesterol. But for those taking narrow-therapeutic-index drugs, multiple medications, or with declining kidney or liver function, the switch needs care. It’s not about distrust-it’s about precision. The FDA and CDC are pushing for better education and monitoring. New guidelines coming in late 2024 will require pharmacists to be part of geriatric medication safety teams. Research is underway to compare brand and generic outcomes in seniors with multiple chronic diseases. Until then, the rule is simple: don’t switch without a conversation. And if you notice a change in how you feel after the switch, speak up. Your life might depend on it.Are generic medications as safe as brand-name drugs for elderly patients?
For most seniors, yes-generic medications are just as safe and effective as brand-name versions. The FDA requires them to contain the same active ingredient, strength, and dosage form, and they must meet strict bioequivalence standards. However, for older adults taking multiple drugs, especially those with narrow therapeutic indexes like warfarin or levothyroxine, even small differences in how the drug is absorbed can matter. These patients need careful monitoring after a switch.
Why do some elderly patients feel worse after switching to generics?
Many seniors report feeling worse after switching due to changes in pill appearance, size, or color, which can trigger anxiety or confusion-especially with memory issues. In some cases, especially with drugs like levothyroxine or warfarin, minor differences in how the generic is formulated can affect absorption in older bodies with slower metabolism or kidney function. While clinical studies don’t show consistent harm, patient reports are real and should be taken seriously. Always report changes in symptoms to your doctor.
Which medications should seniors avoid switching to generics?
The American Geriatrics Society advises caution with drugs that have a narrow therapeutic index-where small changes in blood levels can cause serious side effects. These include warfarin (blood thinner), levothyroxine (thyroid hormone), digoxin (heart medication), phenytoin (seizure control), and lithium (mood stabilizer). Automatic substitution without close monitoring is not recommended. Always ask your doctor if your specific drug falls into this high-risk category.
How can I tell if my generic medication is working the same way?
Pay attention to how you feel. If you notice new symptoms-like fatigue, dizziness, heart palpitations, weight changes, or confusion-after switching, write them down and call your doctor. For certain drugs, like warfarin or levothyroxine, your provider may order blood tests (INR or TSH levels) to check if the dose is still right. Don’t wait for symptoms to get worse. Early detection can prevent hospitalization.
Can over-the-counter drugs interact dangerously with generics?
Absolutely. Many seniors take OTC pain relievers, sleep aids, or cold medicines that contain the same active ingredients as their prescription generics-like acetaminophen or ibuprofen. Taking both can lead to dangerous overdoses. For example, 45% of acetaminophen use in seniors is excessive, raising the risk of liver damage. Always check labels and bring all your medications-prescription and OTC-to your pharmacist for a review.
What should I do if my pharmacy switches my medication without asking?
You have the right to refuse a generic substitution. Ask your pharmacist: “Is this a substitution, or did my doctor prescribe the generic?” If it was changed without your knowledge, you can ask for the brand name instead, especially if you’ve had problems before. Some insurers require prior authorization for brand drugs in high-risk cases-your doctor can help with that. Never stop taking your medication without talking to your provider first.




Generics saved my mom’s life-literally. She was skipping doses because she couldn’t afford Lipitor, and then she started having chest pains. Switched to generic, doctor monitored her INR and cholesterol, and now she’s stable. Don’t fear generics-fear silence. Talk to your pharmacist.
My grandma took Synthroid for 20 years-same white oval pill. Then one day, BAM-blue capsule. She cried. Thought they’d swapped her for a placebo. Turned out the generic dissolved slower. Took three weeks of blood tests, two pharmacy visits, and a handwritten note from her endocrinologist to get the brand back. She still keeps the old bottle on her nightstand like a relic. Sometimes, familiarity is the only medicine that doesn’t need a prescription.
As a geriatric pharmacist, I’ve seen this a hundred times. The problem isn’t the generic-it’s the handoff. No one explains the switch. No one shows the pill. No one asks, ‘How are you feeling?’ If you’re on warfarin or levothyroxine, ask for a TSH or INR check two weeks after the switch. It’s not paranoia-it’s protocol. And yes, if your pill looks different, it’s okay to say ‘I want the one I’ve been on.’ You’re not being difficult-you’re being smart.
Ugh generics. My uncle took some cheap thyroid junk and started hallucinating. Ended up in the ER. They said it was ‘just a difference in fillers.’ Like that’s a good excuse. I’m not paying $600 extra a year, but I’m not letting my family turn into science experiments either.
It’s worth noting that bioequivalence studies for generics are conducted on healthy young adults-never on 82-year-olds with CKD stage 3 and polypharmacy. The FDA’s standards are legally sound but clinically insufficient for our aging population. Until the regulatory framework adapts, the burden of safety falls on the patient, the family, and the overworked pharmacist.
Generics are capitalism’s quiet genocide. We optimize for cost, not cognition. Seniors aren’t data points-they’re people who remember their mother’s face, not their pill’s color. If your algorithm can’t handle that, maybe it shouldn’t be deciding your meds.
Have you ever wondered why the FDA allows generics to differ in fillers? Because Big Pharma owns the FDA. The same companies that make brand names also make generics-they just hide the formula under a different label. Look at the patent filings. The ‘inactive ingredients’? They’re engineered to delay absorption just enough to make you think it’s working-until your body rebels. This isn’t medicine. It’s surveillance with a pill bottle.
I get it. I really do. My dad switched to generic warfarin and started bleeding out his gums. We thought it was just aging-until his INR hit 8.7. We went back to brand. He’s fine now. But here’s the thing: the pharmacist didn’t even ask if he’d been on brand before. No warning. No follow-up. Just a new bottle. That’s not efficiency-that’s negligence. If you’re switching, demand a conversation. Not a transaction.
Oh please. You’re all acting like generics are some kind of poison. My aunt takes 11 pills a day-including generics for everything-and she’s 89 and still gardening. You people treat seniors like fragile porcelain dolls. They’re not. They’ve lived. They’ve survived. A little pill change won’t kill them. Stop infantilizing old people.
generics r fine… unless u r on warfarin. then u r basically playing russian roulette with your blood. my nana had a stroke after switching. the doc said ‘it’s just a diffrent dye’… like that fixes a stroke. lol. no. no it dont.