Why Generic Combination Products Improve Patient Compliance

When you’re managing a chronic condition like diabetes, high blood pressure, or COPD, taking your meds isn’t just about popping pills. It’s about remembering when, how, and why-every single day. And when you’re juggling multiple medications, each with its own schedule, device, or technique, it’s easy to slip up. That’s where generic combination products come in. They don’t just cut costs-they make treatment simpler, safer, and more doable for real people living with long-term health issues.
What Exactly Are Generic Combination Products?
A combination product brings together two or more types of medical components into one unit. Think insulin pens-where the drug (insulin) is built into a pre-filled, easy-to-use injector. Or drug-eluting stents, which are tiny metal mesh tubes that release medicine directly into an artery after placement. These aren’t just pills in a bottle. They’re engineered systems: drug + device, or drug + biologic, working as one. Generic versions of these products copy the original brand-name combination product exactly-same active ingredients, same delivery mechanism, same performance. The FDA requires them to match the brand in every way that matters: dose accuracy within 5%, failure rate under 0.1%, and bioequivalence within 80-125% of the original. The only difference? Price. You might get a generic version of an insulin pen, a patch for nicotine replacement, or an inhaler for asthma-all designed to work just like the brand, but at 30-80% less cost. And that’s where the real win for patients begins.How Combination Products Boost Adherence
People don’t skip meds because they’re lazy. They skip them because it’s hard. Taking three separate pills at different times of day? That’s a recipe for forgetting. Using a vial and syringe for insulin? That’s intimidating for older adults or people with shaky hands. Inhaling from a multi-dose inhaler correctly? It takes practice-and most people don’t get it right the first time. Combination products remove those barriers. A single device does it all:- No more counting pills
- No more mixing drugs
- No more assembling parts
The Cost Advantage That Keeps People on Track
Even the best-designed treatment won’t work if patients can’t afford it. The FDA reports that 23.4% of patients skip doses because of cost. That’s more than one in five. For chronic conditions, that means worsening symptoms, more ER visits, and higher long-term healthcare costs. Generic combination products fix that. They offer the same clinical results as brand-name versions but at a fraction of the price. A single generic insulin pen can cost $25 instead of $120. A generic asthma inhaler might be $15 instead of $70. That’s not a small difference-it’s the difference between taking your medicine and skipping it. And here’s something surprising: patients who start on generic medications are 8.7 percentage points more likely to stick with their regimen than those who start on brand-name drugs. Why? Because when cost is no longer a barrier, people feel less guilt, less stress, and more control over their health.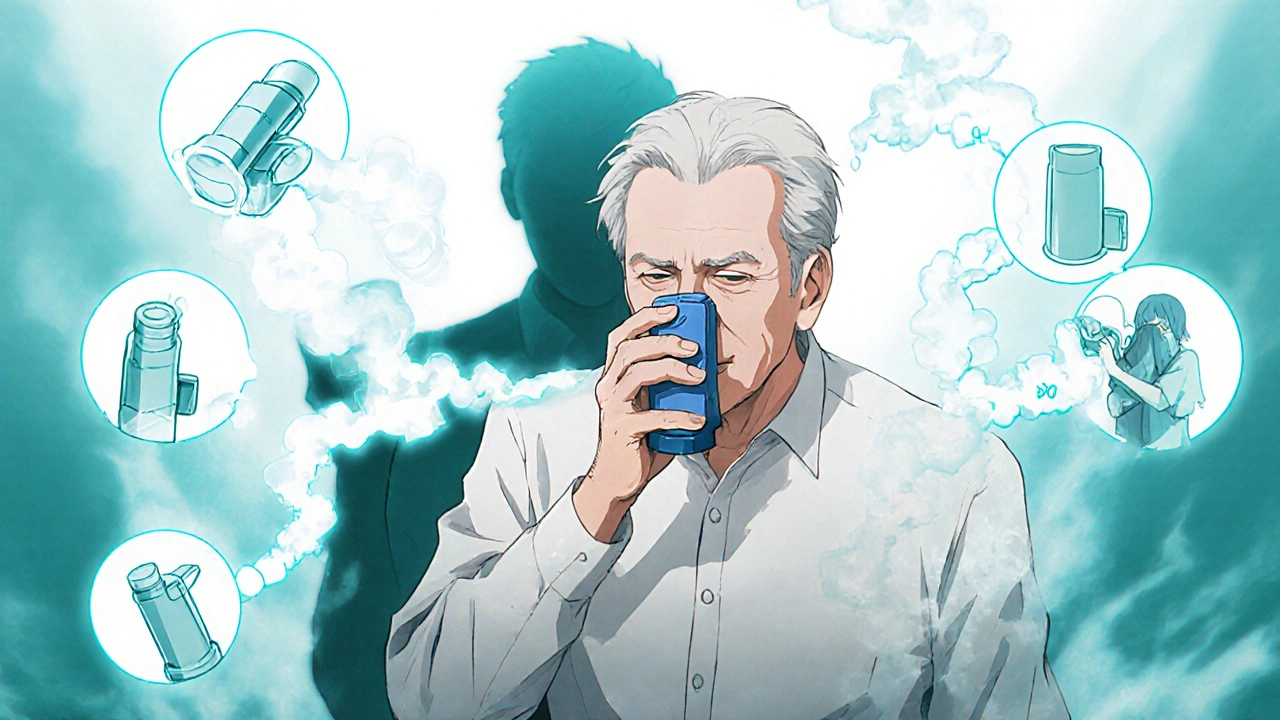
Real Stories Behind the Numbers
On Reddit’s r/Diabetes community, one user wrote: “I used to carry a vial, syringes, alcohol wipes, and a cooler. I missed doses because I didn’t have time to prep. Switching to the prefilled pen cut my dosing errors from 3-4 per week to almost zero.” Another patient with COPD shared on PatientsLikeMe: “I got switched to three different generic inhalers in a year. Each one felt different. I had to relearn how to breathe in. I missed doses until my pharmacist sat with me and showed me the right way.” These stories aren’t outliers. They’re common. And they show something important: the device matters as much as the drug.Where Generic Combination Products Fall Short
The biggest problem isn’t the product-it’s the system. Pharmacies often substitute generic versions without telling patients. That’s legal. But if your inhaler changes from one generic to another, and the button pressure, spray timing, or mouthpiece shape is slightly different, you might not realize you’re using it wrong until you’re short of breath. Dr. Sarah Ibrahim from the FDA says: “Patients may be switched to multiple generics of the same brand name product over the course of a year, which can add to the confusion.” That’s especially true for complex devices like auto-injectors or inhalers. Avalere Health found that 32% of patients who switched generics didn’t get proper retraining. That’s a huge risk. A device that’s 95% the same can still cause 100% non-adherence if the user doesn’t know how to use it.
How to Make Generic Combination Products Work for You
You don’t have to accept confusion as part of the process. Here’s what actually helps:- Ask your pharmacist-every time you get a refill. “Is this the same device as last time?” If it looks different, ask for a demo.
- Request training. Simple patches need 5-10 minutes. Auto-injectors and inhalers need 20-30. Most pharmacies offer this for free.
- Use visual guides. Many generic manufacturers now include QR codes linking to video tutorials. Scan them.
- Stick with one pharmacy. They’ll track your device history and flag changes before you even notice.
- Bring your device to appointments. Don’t just say “I take my pills.” Show your doctor your inhaler. Let them watch you use it.
The Future Is Already Here
The global market for combination products hit $127.5 billion in 2022 and is projected to nearly double by 2030. Diabetes, heart disease, and asthma are the biggest drivers-and generics are catching up fast. New FDA guidance released in June 2023 is pushing for clearer standards on how generic combination products must match the original device function. That means fewer surprises at the pharmacy. And the next wave? Smart combination products. Some new generics now include Bluetooth-enabled inhalers that track when you use them and send reminders to your phone. That’s not science fiction-it’s happening now.Bottom Line: Simpler, Cheaper, Better
Generic combination products aren’t a compromise. They’re an upgrade. They take the clinical benefits of advanced drug-device systems and make them accessible to everyone-not just those who can afford the brand name. The data is clear: fewer pills, fewer mistakes, lower cost, and better outcomes. But only if patients understand how to use them. The real advantage isn’t in the chemistry. It’s in the care. Talk to your pharmacist. Ask questions. Don’t assume the new box is the same as the old one. And if you’re struggling, speak up. Your adherence isn’t just about willpower-it’s about design, support, and access.Generic combination products are one of the most powerful tools we have to turn good treatment plans into real, lasting health.
Are generic combination products as effective as brand-name ones?
Yes. The FDA requires generic combination products to prove they’re bioequivalent to the brand-name version in terms of active ingredients and performance. That means the drug releases at the same rate, the device delivers the same dose with the same accuracy, and the failure rate is below 0.1%. They’re not cheaper because they’re weaker-they’re cheaper because they don’t carry brand-marketing costs.
Can I be switched to a different generic version without warning?
Yes, pharmacies can substitute generic versions without notifying you, as long as they’re FDA-approved. But if the device changes-like a different inhaler design or auto-injector button-you may need retraining. Always check the device when you pick up your prescription. If it looks or feels different, ask your pharmacist to show you how to use it.
Why do some people say generic inhalers don’t work as well?
It’s rarely about the drug. The active ingredient is the same. The issue is the delivery device. Different generics may have slightly different spray timing, mouthpiece shape, or button resistance. If you’re used to one brand and suddenly get another, you might inhale too fast, too slow, or not deeply enough. That’s why training matters. A 15-minute demo can fix most of these problems.
Do generic combination products cost less because they’re lower quality?
No. Generic manufacturers must meet the same strict FDA standards as brand-name companies. The cost difference comes from not paying for advertising, clinical trials, or patent protection. The drug and device are built to the same specifications. In fact, many generics are made in the same factories as the brand-name versions.
How do I know if my combination product is generic?
Look at the label. Generic products will list the active ingredients (same as the brand) but won’t have the brand name. Instead, they’ll say “generic for [Brand Name]” or list the manufacturer’s name. The packaging might look different, but the drug inside is identical. If you’re unsure, ask your pharmacist to confirm.
What should I do if I experience side effects after switching to a generic?
Side effects from switching are rare but can happen. They’re usually due to differences in inactive ingredients (like dyes or preservatives) or incorrect device use-not the active drug. If you notice new symptoms after a switch, document them and contact your doctor. Don’t stop taking your medication without advice. Your pharmacist can help determine if it’s a device issue or a reaction to the generic.
Are generic combination products covered by insurance the same way as brand-name ones?
Usually, yes-and often better. Insurance plans typically place generics in lower cost tiers, meaning you pay less out of pocket. Some plans even require you to try a generic before approving the brand-name version. Always check your plan’s formulary, but in most cases, generics are the preferred and more affordable option.



Generic combo products? Sure they're cheap but who's really testing these things long term? I've seen people get switched to different generics every month and end up in the ER because the inhaler felt 'off' but no one told them to relearn how to use it. The FDA says it's fine but the real world ain't a lab
It's not about the drug. It's about the device. And the training. And the consistency.
Let’s break this down statistically: 15–25% adherence increase? That’s impressive, but only if you control for patient education, pharmacy counseling, and baseline health literacy-which most studies don’t. The real driver isn’t the combo product, it’s the accompanying behavioral intervention. The FDA’s bioequivalence standards? Fine for pills. But for inhalers with 0.05mL variance in spray timing? That’s a clinical gamble. And don’t get me started on the fact that 32% of patients get zero retraining after a switch. This isn’t progress-it’s cost-shifting with a shiny label.
They’re not generics-they’re Trojan horses. Big Pharma owns the generic manufacturers too. You think they’re saving you money? They’re just repackaging the same supply chain with a different label. And the Bluetooth inhalers? That’s not innovation-it’s surveillance. Your medication habits are being tracked, sold, monetized. The FDA’s ‘new guidance’? A PR stunt. They’re not protecting you-they’re protecting the profit model.
Y'all need to stop overthinking this. I switched to a generic insulin pen last year-used to carry a whole kit like a survivalist. Now? Just pop it in my pocket, click, and go. My numbers are better, my stress is lower, and I’m not broke anymore. My pharmacist showed me how to use it in 5 minutes. No drama. No conspiracy. Just better care. If you're struggling, ask for help. It's free. And yes-it works. Trust the process, not the fear.
Also, if you're using an inhaler wrong, no amount of brand-name magic will save you. Learn. Ask. Scan the QR code. It's literally one tap.
And hey-shoutout to my pharmacist, Lisa. She's the real MVP. 🙌
I’ve been on a generic asthma combo inhaler for 18 months now. I didn’t realize how much I was struggling until I stopped having panic attacks before using it. The device feels smoother, the spray is quieter, and I actually remember to use it because it’s just… easier. I never thought a pill case could change my life, but here we are. Thank you to whoever designed this. And to the pharmacists who take the time to show you how it works-you’re doing holy work.
It’s fascinating how much we overlook the physical interaction between patients and devices-especially when those devices are meant to be simple but end up being confusing because of tiny, unannounced changes in button pressure, spray duration, or mouthpiece shape. I’ve seen elderly patients cry because they thought they were doing something wrong when, in reality, the generic inhaler they got this month had a slightly different aerosol timing than last month’s, and no one told them. And yes, the drug is the same-but the human experience isn’t. We treat these as interchangeable like Lego bricks, but the body doesn’t work that way. It remembers. It adapts. And if we keep switching without guidance, we’re not improving access-we’re creating a new kind of medical trauma. We need mandatory retraining every time the device changes, even if it’s ‘just a generic.’ It’s not extra-it’s essential.
Generic combo products? Sounds like a scam to make pharma look good while patients suffer in silence. I know someone who switched and started having chest pains. They blamed her for 'not using it right.' Turns out the new generic had a different propellant. No one warned her. Now she’s terrified of all inhalers. This isn’t healthcare. It’s roulette with your life.