TRICARE Coverage for Generics: What Military Families Need to Know in 2026

When you’re on TRICARE, your prescription drugs shouldn’t be a mystery. But too many military families find themselves stuck at the pharmacy counter, confused about why a generic medication isn’t covered-or why it costs more than expected. The truth is, TRICARE has one of the most structured, transparent generic drug systems in the U.S. healthcare landscape. And if you know how it works, you can save hundreds, even thousands, of dollars a year.
How TRICARE’s Generic Drug Coverage Works
TRICARE doesn’t just cover generics-it pushes them. In 2025, 92% of all prescriptions filled through TRICARE were for generic drugs. That’s not an accident. It’s policy. The Defense Health Agency designed the program to prioritize cost-effective treatments without sacrificing quality. Generic drugs have the same active ingredients, strength, and dosage as brand-name versions. They’re just cheaper-often 80% to 85% less. And TRICARE makes sure you get them.The system is built on a four-tier formulary:
- Tier 1: Generic formulary drugs - The most affordable option. These are the go-to medications for conditions like high blood pressure, diabetes, and cholesterol.
- Tier 2: Brand-name formulary drugs - Covered, but only if no generic alternative exists or if your doctor requests an exception.
- Tier 3: Non-formulary drugs - These aren’t on the approved list. You can still get them, but only after your doctor proves medical necessity-and even then, approval isn’t guaranteed.
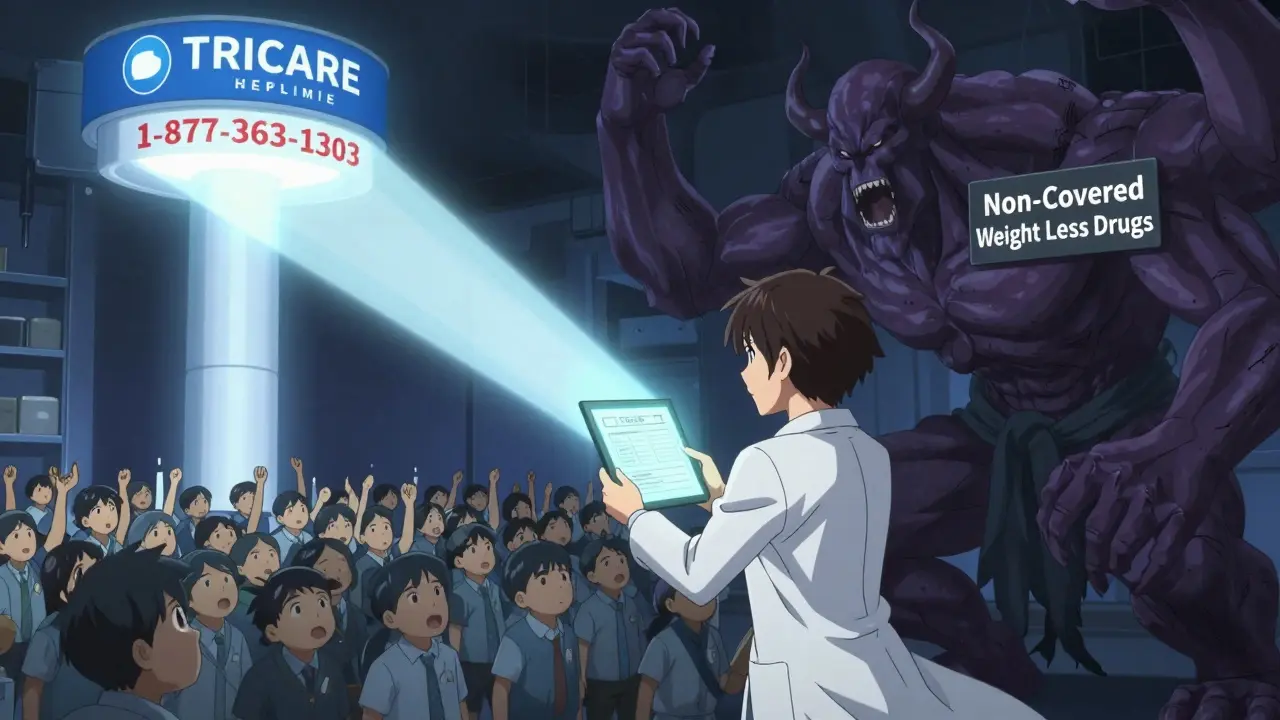
- Tier 4: Non-covered drugs - TRICARE won’t pay for these at all. This includes things like weight loss medications for TRICARE For Life beneficiaries, which were excluded as of August 31, 2025.
Not every generic is automatically covered. About 12% of generic drugs require prior authorization, even if they’re technically on the formulary. That’s because TRICARE uses clinical guidelines to decide which generics are best for each condition. If your doctor prescribes a generic that’s not on the list, you might need to wait 48 to 72 hours for approval. And if the paperwork isn’t complete, it can delay your refill.
Where to Fill Your Prescriptions and How Much It Costs
Where you get your meds matters-big time. TRICARE gives you three options, and each has a different price tag.Military pharmacies are your best bet. If you live near a base or clinic, walk in with your prescription and walk out with your meds-for $0. That’s right. No copay. No deductible. No surprise bills. This is the only place in the entire U.S. healthcare system where you can get a 30-day supply of a generic blood pressure pill without paying a dime. Active duty service members use this option 76% of the time.
TRICARE Home Delivery is ideal for maintenance medications. You can order up to a 90-day supply, which saves you trips to the pharmacy. In 2025, the copay was $13. But starting January 1, 2026, it’s going up to $14. That’s still less than most civilian insurers charge for a 30-day supply. Retirees use this option more than any other-63% of their fills come through home delivery.
Network retail pharmacies like CVS, Walgreens, or Rite Aid are convenient for last-minute refills. The copay for a 30-day supply of a generic formulary drug is $16 in 2025 and 2026. That’s higher than home delivery, but still lower than what most private insurance plans charge. The catch? Not all retail pharmacists know TRICARE rules. If you get pushback, ask to speak to the pharmacist in charge or call the TRICARE pharmacy helpline at 1-877-363-1303.
And here’s something most people don’t realize: if you go to a non-network pharmacy (like a small local drugstore), you’ll pay 50% of the cost after your deductible. That can easily turn a $16 generic into a $50 bill. Always check the TRICARE Formulary Search tool before you go.
The TRICARE Formulary Search Tool: Your Secret Weapon
The single most important tool for TRICARE beneficiaries is the TRICARE Formulary Search on Express Scripts’ website. It’s free, mobile-friendly, and updated every month. You can search by drug name, strength, or even the manufacturer. It tells you:- Is this drug covered?
- What tier is it on?
- What’s the copay at each pharmacy type?
- Does it need prior authorization?
Don’t guess. Don’t assume. Always check. In 2025, a Marine Corps retiree in North Carolina filled a prescription for a generic cholesterol drug at his local pharmacy and got hit with a $48 bill. He later checked the formulary tool and found the same drug was covered as Tier 1 with a $16 copay. He had gone to a non-network pharmacy. He called TRICARE, appealed, and got reimbursed.
Pro tip: If you’re unsure whether your drug is on the formulary, type in the exact name and strength. Don’t use brand names unless you’re comparing. For example, search “lisinopril 10 mg,” not “Zestril.”

What’s Not Covered-and Why
TRICARE doesn’t cover everything. Some exclusions are controversial. The biggest one in 2026 is the ban on weight loss medications for TRICARE For Life beneficiaries. As of August 31, 2025, drugs like semaglutide (Ozempic) and liraglutide (Saxenda) are no longer covered for retirees over 65-even though they’re FDA-approved and widely used for diabetes and obesity. The Defense Health Agency says this was required by the 2024 National Defense Authorization Act. Critics argue it leaves 1.2 million elderly beneficiaries without access to proven treatments.Another gap: generic biologics. These are complex drugs like biosimilar versions of Humira or Enbrel. TRICARE requires 22% more prior authorizations for these than for regular generics. That’s because interchangeability standards are still evolving. If you’re on one of these, expect delays and extra paperwork.
And while TRICARE covers most generics for chronic conditions-like hypertension, diabetes, and asthma-some newer generics for rare diseases aren’t included yet. The formulary updates monthly, so if your drug was removed, it might be because a cheaper, equally effective alternative was added.
How TRICARE Compares to Other Plans
Let’s be clear: TRICARE isn’t perfect. But compared to other government programs, it’s strong.Medicare Part D averages $7-$10 for generics. But Medicare doesn’t have $0 military pharmacies. TRICARE’s $14 home delivery and $16 retail copays are higher-but you get the option to pay nothing at all if you’re near a base. VA benefits are free, but only for veterans with service-connected conditions. TRICARE covers over 9.5 million people, including active duty, retirees, and their families.
Commercial insurers often have higher copays-$20-$40 for generics-and don’t always offer home delivery. Plus, TRICARE’s generic utilization rate (92%) is higher than the national average (90%), meaning the program is more aggressive about pushing affordable options.
TRICARE ranked third in the 2025 Commonwealth Fund Scorecard for government prescription drug access-behind Medicare Advantage but ahead of Medicaid. That’s because it balances cost control with access. In 2025, 94% of beneficiaries said they had no trouble getting their Tier 1 generics. The biggest complaints? Delays in prior authorization and confusion over retail pharmacy pricing.
What to Do If Your Drug Isn’t Covered
If your doctor prescribes a generic that’s not on the formulary, don’t panic. You have options.- Ask your doctor if there’s a similar generic on the formulary. Often, there’s a close alternative.
- If not, they can submit a prior authorization request. The approval rate is 78%-so it’s worth trying.
- Use the TRICARE Formulary Search tool to find a covered substitute. Print the results and bring them to your appointment.
- Call the TRICARE Pharmacy Helpline (1-877-363-1303). They can help you understand your options and even expedite requests.
- If you’re denied, you can appeal. The process takes 10-14 days, but you can get a temporary 30-day supply while you wait.
One retiree in Florida needed a generic for a rare autoimmune condition. It wasn’t on the formulary. Her doctor submitted the paperwork. It took 6 days. She got approved. Her copay? $14 through home delivery. She saved $1,200 a year.
What’s Changing in 2026
The biggest change is the $1 increase for TRICARE Home Delivery-$13 to $14. That’s the first copay hike since 2023. Express Scripts says it won’t affect adherence. Their pilot data showed only a 0.8% drop in fills after similar increases.Other updates:
- 17 new generics were added to the formulary in October 2025, including new versions of common heart and diabetes meds.
- 9 drugs were removed-mostly because better, cheaper alternatives became available.
- By Q3 2026, providers will see real-time cost and coverage info when they e-prescribe. That means fewer surprises at the pharmacy.
- Step therapy will expand to 15 more drug classes by 2027. That means you might need to try a cheaper generic first before getting a pricier one.
- By 2028, TRICARE plans to test pharmacogenomic testing for certain high-risk drugs. This means your genes could determine which medication you get-making treatment safer and more effective.
TRICARE’s pharmacy program is designed to last. The Congressional Budget Office projects it’ll stay financially sound through 2035. As more brand-name drugs lose patents, generic use will climb to 94% by 2030. That could save the program $2.3 billion a year.
Real Stories from Real Beneficiaries
On Reddit, a user named AirForceMom2023 wrote: “Got my lisinopril filled at base pharmacy today, saved $48 versus retail copay.” That’s the kind of story you hear over and over. The $0 military pharmacy is a game-changer.Another retiree on Military.com said: “My generic cholesterol medication costs $14 for 90 days through home delivery-my civilian friends pay $30 for 30 days.”
But not everyone’s happy. A 72-year-old veteran wrote in the TRICARE.mil reviews: “I’ve been on a weight loss drug for two years. August 31, 2025, they cut it off. I gained back 30 pounds. No one told me it was coming.”
That’s the reality. TRICARE saves money. It saves lives. But it’s not always flexible. If you’re on a medication that’s been removed, you need to act fast-talk to your doctor, find alternatives, or appeal.
Final Tips for Managing Your TRICARE Generic Prescriptions
- Always use the TRICARE Formulary Search tool before filling a prescription.
- Use military pharmacies when you can-$0 copay is unbeatable.
- For maintenance meds, choose home delivery. It’s cheaper and more convenient.
- Keep a printed copy of your formulary status for each medication.
- Call 1-877-363-1303 if you’re confused. The helpline handled 1.2 million calls in 2025.
- Check your formulary every 3 months. Changes happen monthly.
- Don’t assume your doctor knows TRICARE’s rules. Ask them to check the formulary with you.
TRICARE’s generic drug coverage isn’t perfect. But it’s one of the most efficient systems in the country. If you use it right, you’ll pay less, get better care, and avoid surprise bills. And that’s worth knowing.
Are all generic drugs covered by TRICARE?
No. Only generics on the TRICARE Formulary are covered. About 12% of generic drugs require prior authorization, even if they’re technically generics. Always check the TRICARE Formulary Search tool to confirm coverage.
What’s the copay for generics at military pharmacies?
$0. All covered generic and brand-name drugs are free at military pharmacies for all TRICARE beneficiaries, including active duty, retirees, and their families.
Why is my generic drug not covered?
Your drug may not be on the TRICARE Formulary, or it may require prior authorization. Some generics are excluded because a cheaper, equally effective alternative exists. Others, like weight loss drugs for TRICARE For Life beneficiaries, were removed by federal mandate as of August 31, 2025.
Can I get my generic medication through home delivery?
Yes. TRICARE Home Delivery offers 90-day supplies of generic formulary drugs. The copay is $14 as of January 1, 2026. It’s the most cost-effective option for maintenance medications like blood pressure or diabetes pills.
What should I do if my pharmacy says my drug isn’t covered?
Ask the pharmacist to verify coverage using the TRICARE Formulary Search tool. If they say it’s not covered, call the TRICARE Pharmacy Helpline at 1-877-363-1303. Sometimes retail staff aren’t trained on TRICARE rules. You may also ask your doctor to submit a prior authorization request.
Are there any drugs TRICARE completely refuses to cover?
Yes. TRICARE does not cover certain non-formulary drugs, including weight loss medications like semaglutide (Ozempic) for TRICARE For Life beneficiaries as of August 31, 2025. Some experimental drugs, cosmetic medications, and over-the-counter drugs are also excluded.


This is why America is falling apart. We give free meds to everyone but expect soldiers to die for it. Meanwhile in Nigeria, we pay for our own pills or die. TRICARE is a luxury. You people don't even know how good you have it.
12% of generics require prior auth thats still too high. The formulary is a mess. You think $0 at military pharmacies is great until you live 200 miles from one. And dont get me started on the weight loss ban. This isnt healthcare its rationing with a flag on it
If you're reading this and you're on TRICARE, you're winning. Seriously. Most people in this country pay more for one prescription than you pay for a year of meds. Use the formulary tool. Call the helpline. Don't let a pharmacist's ignorance cost you. You've got a system that works. Use it. You earned it.
I'm from India. We don't have this. My cousin in Delhi pays $80 a month for a blood pressure pill that costs $14 here. I showed him this post. He cried. You don't realize how lucky you are. This isn't perfect but it's better than most of the world.
Just filled my 90 day supply of metformin at home delivery. $14. My neighbor paid $67 at CVS. TRICARE saved my life. Dont complain. Use the tool. Call the number. This is how it's supposed to work.
The data presented is statistically robust, with a 92% generic utilization rate, which exceeds the national average. However, the exclusion of GLP-1 agonists for TRICARE For Life beneficiaries constitutes a clinically significant gap in therapeutic equity, particularly given the comorbidity burden in the elderly veteran population. The prior authorization burden for biosimilars remains disproportionately high relative to clinical guidelines. Furthermore, the projected $2.3 billion annual savings by 2030 is predicated on assumptions regarding patent expirations that may be subject to regulatory delay.
U.S. is so weak. We in Nigeria we pay for our medicine or die. You people get free pills and still complain. This is why your country is broken. No respect for sacrifice. You think $0 is good? We pay $50 for insulin. You are spoiled. TRICARE is a joke. We have no such thing.
The formulary search tool is your best friend. I used to hate calling the helpline until I found out they can override a pharmacy's mistake. I got my generic albuterol covered after a 3 day wait. Don't give up. This system works if you fight for it
I just checked my meds. My cholesterol pill is Tier 1. $0 at the base. $14 at home. $16 at CVS. I'm saving over $500 a year. And I didn't even have to fight for it. This is the only healthcare system I've ever been in where I didn't get billed for breathing.