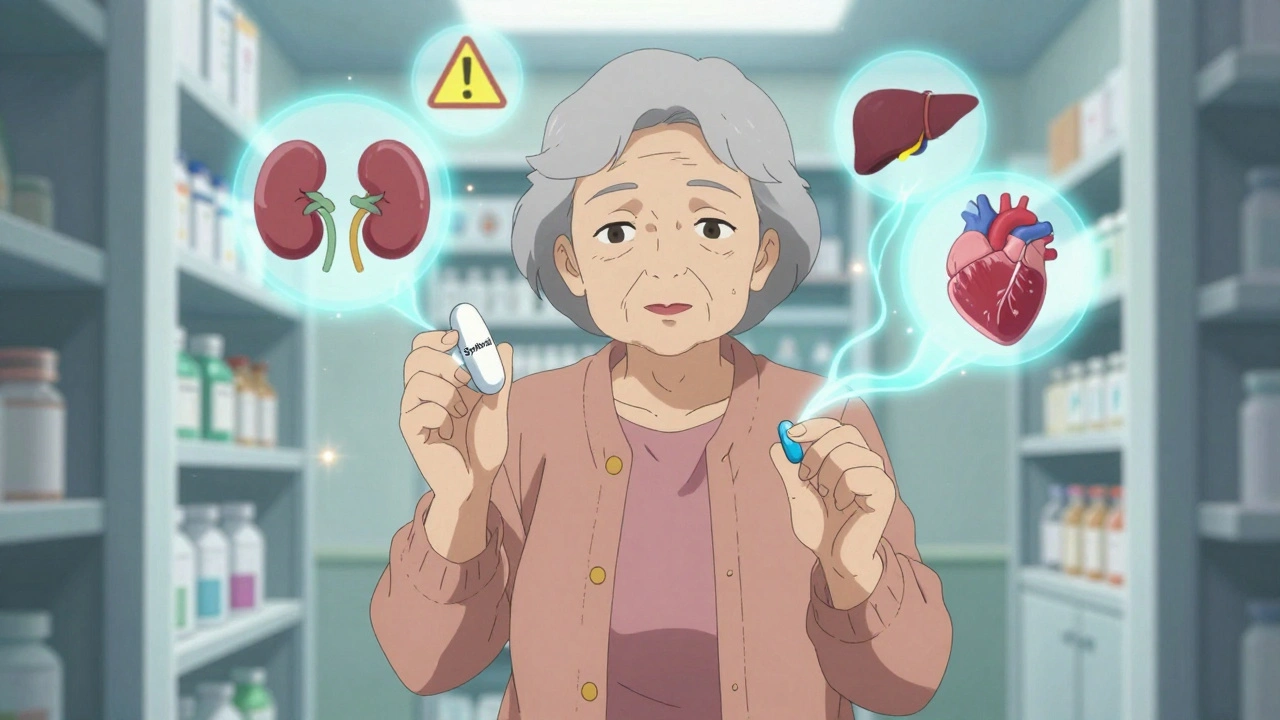
Elderly patients often switch to generic medications to save money, but age-related changes in metabolism, kidney function, and polypharmacy can make these switches risky. Learn which drugs need extra caution and how to stay safe.
Elderly Patients: Medication Safety, Side Effects, and Common Health Risks
When you’re over 65, your body processes drugs differently—and that changes everything. Elderly patients, older adults who often take multiple medications for chronic conditions. Also known as senior citizens, they’re at higher risk for harmful drug interactions, mistaken diagnoses, and side effects that look like normal aging. A fall isn’t just a slip—it could be akathisia from an antipsychotic. Confusion isn’t just dementia—it might be steroid-induced psychosis. Fatigue isn’t just getting older—it could be low blood sugar from diabetes meds or kidney damage from antibiotics. The line between aging and adverse drug reactions is thin, and too often, doctors miss it.
Many elderly patients are on blood thinners, medications like warfarin or DOACs that prevent clots but increase bleeding risk—and that makes dental work, minor injuries, or even brushing too hard dangerous. Then there’s corticosteroids, powerful anti-inflammatories that can cause stomach ulcers when mixed with NSAIDs like ibuprofen. Combine that with SSRI side effects, common antidepressants that cause sexual dysfunction, weight gain, and withdrawal symptoms, and you’ve got a perfect storm. Add in supplements like ashwagandha that can spike thyroid levels, or CoQ10 that messes with blood pressure meds, and it’s no wonder so many seniors end up in the ER.
It’s not just about what you take—it’s about how you take it. Five simple rules can prevent 80% of medication errors: check the name, dose, timing, route, and your own identity. Too many elderly patients take the wrong pill because labels are too small, or they’re confused by multiple prescriptions. Insurance often pushes combo pills to cut costs, but sometimes, two separate generics are safer and cheaper. And don’t assume a generic works the same just because it’s labeled the same—your brain matters too. Placebo and nocebo effects are real, especially when you’ve been told a drug is "weak" or "cheap."
What you’ll find below isn’t theory. These are real stories from elderly patients who survived dangerous mistakes—and the guides that helped them. From spotting restless legs vs. medication-induced akathisia, to knowing when to call poison control after a child’s overdose (yes, it happens when meds are left within reach), to understanding why your dentist needs to know about your blood thinners—every post here is about keeping older adults safe, clear-headed, and in control of their health.