Shellfish Allergy: Cross-Reactivity and How to Eat Out Safely

If you have a shellfish allergy, eating out isn’t just risky-it’s unpredictable. One bite of shrimp scampi, a splash of broth in your stir-fry, or even fried food cooked in the same oil as crab can trigger a reaction. And it’s not just about avoiding the obvious. The real danger lies in hidden cross-reactivity and misunderstood kitchen practices. This isn’t theoretical. In 2022, nearly 70% of people with shellfish allergies reported at least one accidental exposure while dining out. A quarter of those cases required epinephrine. You don’t need to live in fear, but you do need to know what you’re up against.
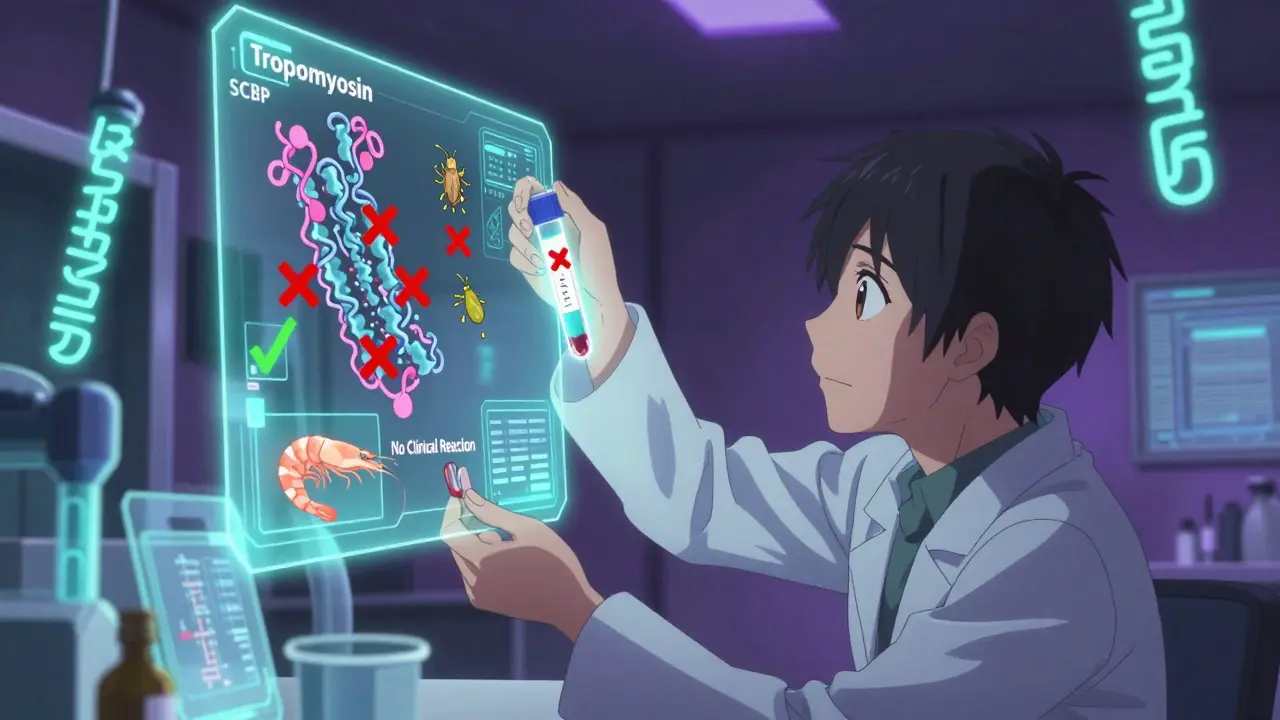
What Exactly Are You Allergic To?
Shellfish allergy isn’t one thing. It’s mostly about a protein called tropomyosin. This protein is found in shrimp, crab, lobster, and crawfish-and it’s incredibly stubborn. Unlike some allergens that break down when cooked, tropomyosin stays active even after boiling, frying, or grilling. That’s why you can’t rely on cooking to make shellfish safe. It doesn’t work.Tropomyosin is also the reason you can’t assume you’re only allergic to one type of shellfish. If you react to shrimp, there’s a 75% chance you’ll react to crab or lobster too. That’s because these crustaceans share nearly identical versions of tropomyosin. But mollusks like clams, oysters, scallops, and mussels? They’re different. Only 15-20% of people allergic to shrimp or crab react to mollusks. That’s a big deal. Some people who think they’re allergic to all shellfish can actually eat oysters safely-if they’ve been tested properly.
And here’s the twist: you might test positive for shellfish allergy even if you’ve never eaten it. Dust mites and cockroaches have proteins that look a lot like tropomyosin. About half of people allergic to dust mites show IgE antibodies to shrimp or crab in blood tests. But they don’t have symptoms. This is called cross-reactivity without clinical allergy. Without component-resolved testing (which checks for specific proteins like tropomyosin and SCBP), you could be avoiding entire food groups unnecessarily.
How Testing Works-And Why It Matters
Standard skin prick or blood tests use whole shellfish extracts. They’re easy, but they’re messy. They can’t tell the difference between a real allergy and a false positive from dust mites. That’s why allergists now recommend component-resolved diagnostics. These tests look at individual proteins, especially tropomyosin and sarcoplasmic calcium-binding protein (SCBP). When both are positive, the chance of a true shellfish allergy jumps to 92%. If only tropomyosin is positive, and you’ve never had symptoms, you might be fine.Oral food challenges are still the gold standard. If your test results are unclear, an allergist might have you eat a tiny, controlled amount of shellfish under supervision. It’s the only way to be 100% sure. Many people avoid shellfish for years based on a false positive, only to find out later they could have eaten it safely. That’s not just inconvenient-it’s emotionally exhausting.
Where the Real Danger Hides: Dining Out
You might think avoiding seafood restaurants is enough. But 87% of reactions happen in places that serve shellfish-not necessarily the ones that specialize in it. Think Chinese, Thai, or Japanese restaurants. Why? Because shellfish is hidden in sauces, broths, and seasonings. Fish sauce? Often made with shrimp. Oyster sauce? Full of shellfish. Even fried rice might be cooked in oil that previously fried shrimp.A 2020 study found that 41% of shellfish allergy reactions occurred in Asian restaurants. Servers often don’t know what’s in the sauces. Kitchen staff might say, “We don’t use shrimp in that dish,” but they’re wrong. The broth was made with shrimp stock. The wok wasn’t cleaned between orders. The fryer? Shared with tempura shrimp.
And it’s not just ethnic restaurants. Even casual chains like pizza places or burger joints might use shellfish in their seasoning or fryer oil. A 2019 study showed that 63% of crustacean reactions from dining out came from cross-contact in shared fryers. One person ate chicken fingers at a diner and went into anaphylaxis-because the fryer had been used for shrimp earlier that day.
How to Eat Out Without Risking Your Life
You don’t have to give up dining out. You just need a system.- Call ahead. Don’t wait until you get there. Call 24 hours in advance. Ask to speak to the chef or manager. Explain you have a life-threatening shellfish allergy. Ask if they have a separate fryer, clean prep surfaces, and dedicated utensils.
- Use a chef card. Print or carry a card written in clear, simple language. Include the allergens you react to and what to avoid: “I am allergic to shrimp, crab, lobster, and any product containing them. Cross-contact with these foods can cause anaphylaxis. Please use clean utensils, pans, and fryers.” The Food Allergy Research & Education (FARE) card is available in 15 languages.
- Avoid shared fryers. If they fry fish, chicken, and shrimp in the same oil, walk away. No exceptions.
- Speak to the chef, not just the server. Servers are not trained to know ingredients in sauces or broths. A 2023 study found only 37% of servers could correctly identify shellfish ingredients in common dishes.
- Use apps like AllergyEats or Nosh List. These apps let users report which restaurants are safe. Nosh List has data from over 120,000 users. Look for places with high ratings from people with shellfish allergies.
It takes time to get good at this. Most people need 6 to 12 months of trial and error to learn what works. Start small. Try a local restaurant with a reputation for transparency. Bring your own condiments if you’re unsure. Be polite but firm. You’re not being difficult-you’re protecting your life.

The New Hope: Emerging Treatments
There’s good news on the horizon. In January 2024, a Phase 2 clinical trial at Mount Sinai showed that peptide immunotherapy for shrimp allergy led to 70% of participants becoming desensitized. They could eat small amounts without reaction. It’s not a cure yet, but it’s a major step. This therapy uses tiny, modified pieces of the tropomyosin protein to retrain the immune system-without triggering a full-blown reaction.Also in 2024, the FDA approved a new diagnostic panel called ImmunoCAP ISAC 112. It checks for 112 allergens at once, including tropomyosin, SCBP, and dust mite proteins. It can now tell you whether your positive test is from a real shellfish allergy or just dust mite cross-reactivity. This means fewer people will unnecessarily avoid shellfish.
AI tools are starting to help too. Apps like AllergyMapper (beta, launched March 2024) scan restaurant menus and flag hidden shellfish ingredients. It’s not perfect yet-but it’s getting better.
What You Can Do Today
If you’re newly diagnosed, get component-resolved testing. Don’t assume you’re allergic to all shellfish. If you’ve been avoiding everything for years, talk to your allergist. You might be able to eat scallops or clams safely.If you’re a parent of a child with this allergy, teach them to speak up. Practice with role-playing. “I have a shellfish allergy. I need a clean pan.” Make sure their school has an emergency plan and epinephrine on hand.
If you’re dining out, never rely on a server’s word. Ask for the chef. Bring your card. Avoid fried foods unless you know the oil is clean. And always carry two epinephrine auto-injectors. One might not be enough.
Shellfish allergy is serious, but it’s manageable. You don’t have to give up eating out. You just have to be smart, prepared, and persistent. The science is on your side. The tools are getting better. And you’re not alone.
Can you outgrow a shellfish allergy?
Unlike allergies to milk or eggs, shellfish allergy is rarely outgrown. Only about 10-15% of people lose their sensitivity over time. Most will have it for life. That’s why ongoing caution and proper testing are essential.
Is it safe to eat imitation crab if I’m allergic to shellfish?
No. Imitation crab is usually made from pollock fish, but it often contains shellfish extracts like crab flavoring or shellfish-derived additives. Even trace amounts can trigger a reaction. Always read labels carefully and avoid it unless it’s explicitly labeled as shellfish-free and made in a dedicated facility.
Why do some people test positive for shellfish but never react?
This is due to cross-reactivity with dust mites or cockroaches. Their proteins look similar to tropomyosin in shellfish. Blood tests detect these similar proteins, but the immune system doesn’t react when you eat shellfish. Component-resolved testing can tell the difference. If your sIgE is only to dust mite proteins and not to shellfish tropomyosin, you’re likely not allergic to shellfish.
Can I eat at a sushi restaurant?
It’s risky. Many sushi restaurants use fish sauce, shrimp paste, or shellfish in their sauces and broths. Even rice might be seasoned with shellfish-derived ingredients. Sashimi (raw fish) is usually safe-but only if the knife, cutting board, and prep area are completely clean. Always ask the chef and bring a chef card. Avoid any dish with “spicy mayo,” “eel sauce,” or “tempura” unless you’re certain it’s shellfish-free.
Do I need to avoid iodine or contrast dye if I have a shellfish allergy?
No. This is a myth. Shellfish allergy is not related to iodine. Iodine is not an allergen-it’s a mineral. Contrast dye reactions are caused by the chemical structure of the dye, not shellfish proteins. People with shellfish allergies are no more likely to react to contrast dye than anyone else. Don’t avoid necessary medical procedures because of this outdated belief.
Are there any restaurants that are reliably safe for shellfish allergies?
Some chains have strong allergen protocols. Chipotle, Panera Bread, and Sweetgreen use digital allergen menus with 98% accuracy. They train staff, separate prep areas, and update menus in real time. Independent restaurants vary widely. Use apps like AllergyEats and check recent reviews from others with shellfish allergies. Look for places that say they have a “dedicated fryer” or “allergen-free kitchen zone.”
What should I do if I have a reaction while dining out?
Use your epinephrine auto-injector immediately. Don’t wait to see if symptoms get worse. Call 911. Even if you feel better after the shot, you still need emergency care-symptoms can return hours later. Tell the staff what happened and ask them to save the food you ate. It can help doctors identify the trigger.


Shared fryers are a death sentence. Walk out if they fry anything seafood-related. No exceptions.
I used to avoid all restaurants until I started carrying that FARE chef card. Made a huge difference. Last month I ate at a Thai place in Austin-the chef came out, checked his stock, and made me a custom dish with a clean wok. Felt seen for the first time.
Let me tell you something-this isn’t just about food. It’s about dignity. Every time you have to explain to a server that ‘no, really, I don’t mean ‘maybe’ or ‘I think’-I mean I WILL DIE if you touch that fryer-you’re not asking for special treatment. You’re asking to live. And that’s not too much to ask. I’ve been there. I’ve had the EpiPen in my hand while a manager shrugged and said ‘we’ve never had a problem before.’ You know what? That’s not a record. That’s a waiting game. Don’t wait for someone else to get it right. You’re the expert on your body. Trust that. Fight for it. And if they don’t get it? Walk out. No guilt. No apology. You’re not being difficult-you’re being alive.
Component-resolved testing changed my life. I thought I was allergic to everything shellfish-until my allergist ran the specific IgE panel. Turns out I only react to tropomyosin. I can eat scallops and oysters safely now. So many people are unnecessarily avoiding food they could enjoy. Please, if you’ve been avoiding shellfish for years, ask your doctor about this test. It’s not just convenient-it’s life-changing.
Let’s be honest-most restaurants are death traps for people with shellfish allergies. The idea that ‘servers know what’s in the food’ is a fantasy. A 2023 study showed only 37% could correctly identify shellfish in sauces. That’s not incompetence-that’s systemic negligence. And don’t get me started on ‘allergen-free zones.’ Most are just marketing buzzwords. The real solution? Mandatory allergen training certified by the FDA, not some third-party vendor. Until then, every time you walk into a restaurant, you’re gambling with your life. And the system? It’s rigged.
I’ve been saying this for years: the entire food industry is lying to us. Why do you think they won’t disclose ‘shellfish-derived flavoring’? Because they don’t want you to know you’re eating crushed crab in your ‘vegetable broth.’ And don’t even get me started on the iodine myth-it’s a distraction tactic by Big Pharma to keep you from questioning why they’re pushing those expensive ‘allergy tests.’ They profit from fear. The truth? They’re poisoning us with hidden allergens and selling us ‘solutions’ to the problems they created. Check the labels. Demand transparency. Or die quietly. Your choice.
Let me tell you something, Americans-your entire approach to food allergies is chaotic. In the UK, we have mandatory allergen labeling on every single ingredient, and restaurant staff are legally required to know what’s in every dish. You people rely on ‘chef cards’ and apps? Pathetic. We have a national database, standardized training, and fines for non-compliance. You think you’re ‘being safe’? You’re just surviving in a broken system. Meanwhile, in London, you can walk into any pub and ask for a shellfish-free meal-and they’ll have one ready. Why? Because we don’t treat your survival as optional.
Just wanted to add a practical note: if you're using AllergyEats or Nosh List, always check the date of the reviews. A place that was safe in 2022 might have changed management or kitchen staff in 2024. I once trusted a 2-year-old review, got sick, and spent three days in the ER. Now I only trust reviews from the last 90 days. Also, don’t forget to check the restaurant’s own allergen page-if they have one. Some chains update theirs daily. It’s not foolproof, but it’s better than guessing.
Just got my first dose of that peptide immunotherapy last week 🥹 I’m not cured, but I ate a shrimp spring roll today… and didn’t die. I cried. Not because I was scared-I cried because I realized I hadn’t tasted shrimp in 14 years. This isn’t just science. It’s hope. And if you’re still avoiding everything? Please, talk to your allergist. The future is here. We just have to reach for it.