Prior Authorization for NTI Drugs: When Insurers Require Brand-Name Medications

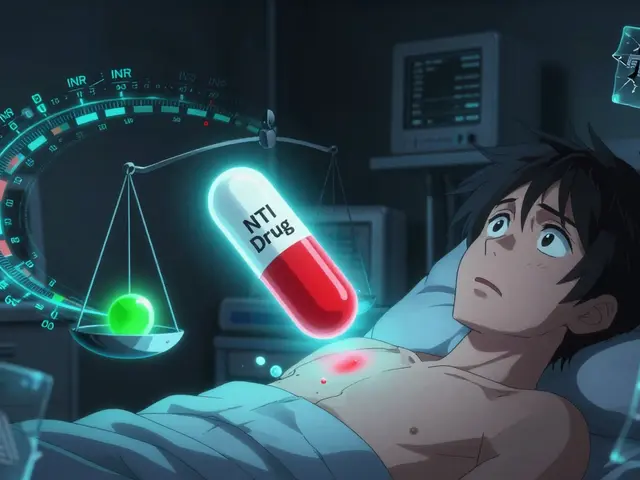
When you’re taking a medication for epilepsy, hypothyroidism, or another serious condition, your life depends on consistency. A tiny change in how your body absorbs the drug can mean the difference between control and crisis. That’s why NTI drugs - narrow therapeutic index drugs - are handled differently by insurers, even when generics are available. Most people assume that if a generic version exists, insurance will push you to use it to save money. But with NTI drugs, that logic doesn’t hold. In fact, many insurers now require you to stay on the brand-name version - not because they’re being expensive, but because the risks of switching are too high.
What Makes an NTI Drug Different?
NTI drugs have a razor-thin margin between a safe, effective dose and a dangerous, toxic one. The FDA defines them as medications where small changes in blood concentration can lead to treatment failure or serious side effects. This isn’t theoretical. It’s life-or-death.
Take levothyroxine, the standard treatment for hypothyroidism. A patient stable on 75 mcg of Synthroid might see their TSH levels spike by 300% after switching to a generic version. That’s not a minor fluctuation - it’s a signal that the body isn’t getting the hormone it needs. For someone with heart disease or a history of arrhythmias, that spike can trigger chest pain, dizziness, or worse.
Same with phenytoin and carbamazepine, two anticonvulsants used for epilepsy. Even slight variations in absorption can cause breakthrough seizures. A 2024 study from the American Academy of Neurology tracked 2,450 epilepsy patients and found that 18.7% experienced preventable seizures after being forced to switch from brand to generic. That’s nearly one in five people having a seizure that could have been avoided.
There are about 37 known NTI drugs on the market, and they’re not rare. They’re essential. That’s why many insurers, including Health Net and some Medicaid programs, explicitly list them as exceptions to standard prior authorization rules - meaning they don’t require you to try the generic first. In fact, they often require you to stay on the brand.
Why Do Insurers Still Require Prior Authorization?
If NTI drugs are so dangerous to switch, why does prior authorization even exist for them? The answer is messy.
Some insurers still apply generic-first policies out of habit, not science. They treat NTI drugs like every other medication. Others use prior authorization as a gatekeeping tool - not to protect patients, but to control costs. They’ll approve brand-name NTI drugs only after you submit lab results, medical history, and proof that the generic failed.
Here’s the problem: that process takes time. The average prior authorization for an NTI drug takes 3.2 business days to process, according to a 2023 study in the Journal of Managed Care & Specialty Pharmacy. For a patient with unstable epilepsy or uncontrolled thyroid levels, three days can mean a hospital visit, an emergency room trip, or a seizure.
And it’s not just delays. Denials happen. One neurologist on Reddit reported that 73% of their levothyroxine brand-name requests were initially denied, even when patients had clear signs of instability. That’s not just frustrating - it’s dangerous.
Meanwhile, some insurers have gotten smarter. Health Net’s policy, updated in 2023, says NTI brand drugs “may be listed on the Formulary at a higher tier and do not require prior approval.” That means if your doctor prescribes Synthroid or Keppra, you get it - no paperwork, no waiting.
State Laws Are Changing the Game
Patients and doctors have been pushing back for years. And it’s working.
By mid-2024, 22 states had passed laws limiting prior authorization for NTI drugs. California’s AB-1428, effective January 1, 2025, is one of the strongest. It bans insurers from requiring prior authorization for an NTI drug if the patient has been stable on the brand-name version and their condition hasn’t changed. No forms. No delays. Just refill.
Eighteen states now require automatic approval if an insurer doesn’t respond within a set time - usually 72 hours. That’s up from just seven states in 2022. Mississippi, North Carolina, and others have also updated their Medicaid rules to exempt NTI drugs from step therapy requirements.
The federal government is catching up too. The Improving Seniors’ Timely Access to Care Act, passed by the House in April 2024, requires Medicare Advantage plans to give real-time electronic decisions on prior authorization requests. For NTI drugs, that means no more faxing forms or waiting days for a call back.
Industry analysts predict that by 2026, 75% of commercial insurers will eliminate prior authorization for established NTI drug categories. Why? Because the data is clear: forcing switches increases costs in the long run through ER visits, hospitalizations, and lost productivity.
What Prescribers Need to Know
If you’re a doctor prescribing an NTI drug, you’re not just writing a script - you’re writing a safety plan.
First, document why the brand is necessary. Don’t just say “patient prefers.” Say: “Patient experienced TSH fluctuation of 300% on generic levothyroxine, with symptoms of fatigue and palpitations. Brand-name required for therapeutic stability.”
Second, use electronic prior authorization systems. Paper requests take longer. Fax delays are common. The NCTracks portal in North Carolina and the Gainwell portal in Mississippi are faster - but only if you know how to use them. A 2024 CAQH report found that electronic systems cut processing time by 42% for NTI drugs, though they still take 22% longer than standard requests because of the extra clinical data needed.
Third, know your state’s rules. In some places, you can override prior authorization with a simple note: “Medically necessary for NTI drug.” In others, you need a specific form, lab values, or even a letter of medical necessity.
And don’t underestimate the administrative burden. A 2023 MGMA survey found that physicians spend an average of 16.3 hours per week just managing prior authorizations. That’s nearly two full workdays - time that could be spent with patients.

What Patients Can Do
If you’re on an NTI drug and your insurer denies your brand-name prescription, here’s what to do:
- Ask your doctor to appeal immediately. Most insurers have a fast-track process for NTI drugs if the condition is unstable.
- Request a copy of the insurer’s prior authorization criteria. You have a right to it. If they’re applying generic rules to an NTI drug, that’s often grounds for appeal.
- Check your state’s health department website. Many post lists of NTI drugs exempt from prior authorization.
- Use patient advocacy groups. Patients Rising and the Epilepsy Foundation have templates for appeals and direct lines to insurer case managers.
- Document everything - missed doses, symptoms, lab results. That’s your evidence.
One patient on HealthUnlocked shared that after a grand mal seizure caused by a generic switch, her insurer automatically approved Keppra without prior authorization on the second try. That’s not luck - it’s policy change in action. But she had to fight first.
The Bigger Picture
This isn’t just about pills. It’s about trust. Patients trust their doctors. They trust their medications. When insurers force switches without clinical justification, that trust breaks.
Insurers argue that prior authorization saves money. And yes, it does - in the short term. But when a patient has a seizure, goes to the ER, or ends up hospitalized because their thyroid med wasn’t stable, the cost skyrockets. A 2024 study in the AMCP Journal found that while prior authorization saves health plans $2.3 billion annually, those savings are offset by avoidable complications for NTI drugs.
The real win? Removing barriers for NTI drugs. Not because they’re expensive - but because they’re fragile. The science is clear. The data is clear. And more and more, the law is too.
If you’re on an NTI drug, you deserve consistency. Not paperwork. Not delays. Not guesswork. You deserve the right medication - the one that keeps you safe - without having to prove you need it.
What are NTI drugs?
NTI drugs, or narrow therapeutic index drugs, are medications where small changes in dosage or blood concentration can lead to serious side effects or treatment failure. Examples include levothyroxine for hypothyroidism, phenytoin and carbamazepine for epilepsy, and warfarin for blood clotting. These drugs have a very narrow window between effective and toxic levels.
Why do insurers require prior authorization for brand-name NTI drugs?
Insurers require prior authorization for brand-name NTI drugs to ensure they’re only used when medically necessary - not because of cost preference. While generics are cheaper, switching NTI drugs can cause dangerous instability. Prior authorization allows insurers to review clinical evidence - like lab results or seizure history - before approving the brand-name version.
Can I get a generic version of an NTI drug?
Technically, yes - many NTI drugs have generic versions. But switching isn’t always safe. Studies show that patients on levothyroxine or anticonvulsants often experience unstable blood levels after switching to generics. Many doctors and insurers now recommend staying on the brand if it’s working, especially if you’ve had issues with generics before.
How long does prior authorization for NTI drugs take?
On average, it takes 3.2 business days to process a prior authorization request for NTI drugs. Some insurers offer expedited reviews for urgent cases - especially if the patient has recently had a seizure, hospitalization, or lab result showing instability. In emergency situations, federal Medicaid rules require a 72-hour supply to be dispensed while the request is reviewed.
Which states don’t require prior authorization for NTI drugs?
As of 2025, 22 states have laws limiting or eliminating prior authorization for NTI drugs. California, New York, Illinois, and Washington are among the strongest, with rules that automatically approve brand-name prescriptions if the patient is stable. Eighteen states require automatic approval if insurers don’t respond within 72 hours. Always check your state’s Medicaid or insurance department website for the latest rules.


Wow, this is exactly why I stopped trusting insurance companies. My mom was switched to generic levothyroxine last year-she went from feeling fine to collapsing at the grocery store. TSH levels went from 2.1 to 6.8 in two weeks. They made her fill out six forms just to get Synthroid back. And no, she didn’t ask for it-she was forced into it. This isn’t cost-saving-it’s cruelty with a spreadsheet.
Let’s be real-this whole NTI thing is a pharma scam. Big Pharma pays insurers to keep brand names on the formulary so they can keep charging $500 a pill. Meanwhile, generics are tested just as rigorously-except they don’t have the marketing budget. The FDA’s bioequivalence standards are a joke. 80-125%? That’s a 45% swing! You’d never let someone drive a car with a 45% variance in brake pressure. Why are we letting them do it with brain meds?
As a pharmacist in Mumbai, I see this daily. Even in India, where generics dominate, neurologists insist on brand for phenytoin. Why? Because patients come back with seizures-not because they missed a dose, but because the generic dissolved too fast. We’ve learned the hard way. Science doesn’t care about your country’s currency. What matters is the blood level. And if it’s unstable? That’s not economics-that’s tragedy.
If you’re on an NTI drug, don’t fight the system alone. Talk to your pharmacist-they often have direct lines to insurers and know which forms get approved fastest. Also, ask for a prior auth template from your doctor’s office. Many clinics now have pre-filled ones for levothyroxine and carbamazepine. It cuts the wait from days to hours. And if they deny it? File a complaint with your state’s insurance commissioner. They get hundreds of these every month-and they’re starting to take notice.
So… the government’s gonna save us? LOL. You really think AB-1428 means anything? That’s just theater. The same people who wrote that law also voted to cut Medicaid funding last year. This is all a distraction. They want you to think you’re being protected while they quietly let insurers find loopholes. You think they don’t have a ‘clinical stability’ loophole that’s impossible to prove? Of course they do. You’re not being helped-you’re being managed.
i had a seizure last year after they switched me to generic carbamazepine. i didn’t even know it was a thing. my doc said it was fine. i trusted them. i was in the er for 3 days. now i just beg for synthroid. i don’t care if it costs more. i just want to not die. pls don’t make people go through this.
Bro, I’ve been on levothyroxine for 12 years. Brand only. No issues. But I’ve seen friends switch-big mistake. One guy got dizzy, lost his job. Another had panic attacks. It’s not about money. It’s about your body. You don’t swap out your car’s engine just because a cheaper one exists. Same here. 🙏
They’re lying to you. All of them. Insurers, doctors, even the FDA. The real reason they don’t want generics for NTI drugs? Because the generics are too good. They’re too consistent. And if generics worked perfectly, Big Pharma would lose their monopoly. So they make up this ‘danger’ story to scare you. It’s not about safety-it’s about profit. Wake up.
One tip: if your doctor writes 'NTI drug - medically necessary' on the script, many pharmacies can override the denial right at the counter. No waiting. Just show them the list from your state’s health site. I’ve done it twice. Saved my friend from a hospital trip. Small move. Huge difference.
My wife’s on Keppra. Switched to generic once. Seizure within 72 hours. We had to go to three different pharmacies before one would fill the brand without prior auth. The pharmacist said, 'I’ve seen this too many times. I won’t dispense it unless it’s brand.' That’s the real hero-not the insurer, not the doctor. The pharmacist who knows the stakes.
This whole thing is western privilege. In Nigeria we take whatever is available and survive. Why should we care about 0.05 mg differences? People die from hunger not from generic meds. You think your body is special? Everyone else manages. You just want expensive pills because you can afford to complain
Of course insurers require prior auth. They know if they just approve brand NTI drugs outright, everyone will start asking for it. Next thing you know, everyone wants brand-name ibuprofen. This is how the system works. You want luxury? Pay for it. Don’t blame the insurer for not being your personal pharmacy. You think your thyroid is more important than someone else’s diabetes meds? Wake up.
This entire post is a beautifully constructed narrative of victimhood. You frame NTI drugs as uniquely fragile, but you ignore the fact that every drug has pharmacokinetic variability. The body is not a machine. It’s a chaotic, adaptive system. To treat levothyroxine as sacred and every other drug as disposable is not medical science-it’s pharmaceutical romanticism. The real tragedy? You’ve outsourced your agency to a pill. Your identity is now tied to a brand name. That’s not medical necessity. That’s dependency culture.