Five Essential Rules for Taking Medication Safely

Every year, over a million people in the U.S. end up in the emergency room because of mistakes with their medications. Many of these aren’t accidents-they’re preventable. You might think you’re doing everything right: you take your pills on time, read the labels, and never miss a dose. But if you’re not following the core safety rules, even small oversights can lead to serious harm. The truth is, taking medication safely isn’t just about remembering to swallow your pills. It’s about understanding what you’re taking, why you’re taking it, and how to avoid hidden risks.
Rule 1: Know Exactly What You’re Taking
It sounds simple, but many people don’t know the difference between brand names and generic names. Your doctor might prescribe lisinopril, but the bottle says Zestril. If you don’t recognize both names, you might think you’re getting two different drugs. Look-alike, sound-alike medications cause about 25% of reported medication errors. Insulin and heparin, for example, are often confused because their names and packaging are similar. Always check the generic name on the label. If it’s not clear, ask your pharmacist to write it in big letters. Don’t rely on color or shape alone-medications can change manufacturers, and pills might look totally different even if they’re the same drug.Rule 2: Take the Right Dose for Your Body
One size doesn’t fit all. A dose that’s safe for one person could be dangerous for another. Weight, age, kidney function, and liver health all affect how your body processes medicine. Kids and older adults are especially at risk. For example, a standard adult dose of acetaminophen (Tylenol) is 650-1000 mg every 6 hours. But if you’re over 65 or have liver issues, even 325 mg twice a day could be too much. High-alert medications like warfarin, insulin, or opioids require extra care. Always double-check the dose with your pharmacist, especially if you’re starting a new drug. If your doctor says, “Take one pill,” but the bottle says “Each pill contains 5 mg,” and your prescription says 2.5 mg-you’re being given double what you need. Never assume. Ask.Rule 3: Take It at the Right Time
Timing matters more than you think. Some medicines need to be taken with food to reduce stomach upset. Others need to be taken on an empty stomach so they absorb properly. Blood pressure meds often work best when taken in the morning. Antibiotics like amoxicillin need to be spaced evenly-every 8 hours, not just “three times a day.” Missing a dose by a few hours can reduce effectiveness. For drugs like warfarin, even a 4-hour delay can throw off your blood levels. Use a pill organizer or set phone alarms. But don’t just rely on memory. If you’re on five or more medications, schedule a quarterly medication review with your pharmacist. They’ll spot overlaps, timing conflicts, or doses that don’t make sense together.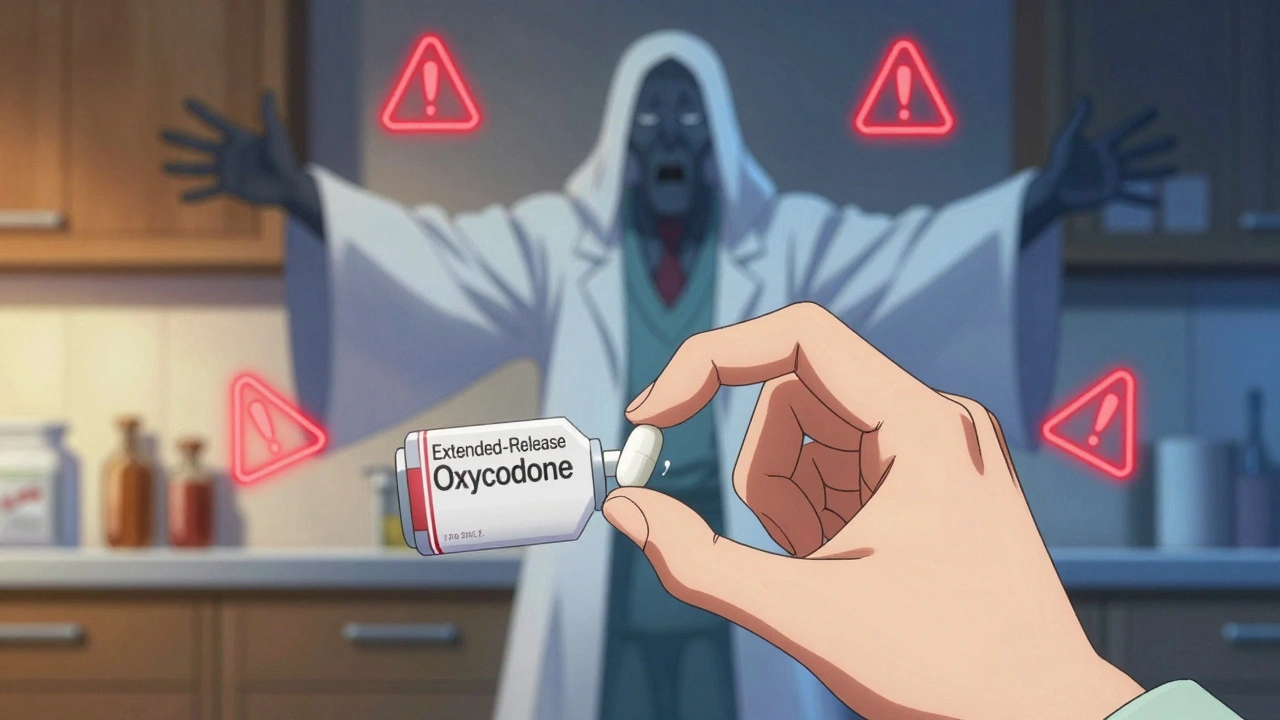
Rule 4: Use the Right Route
You wouldn’t inject a pill into your arm-and yet, people do this by accident. Oral medications meant to be swallowed are sometimes crushed and snorted. Eye drops are accidentally put into ears. Transdermal patches meant for skin are placed on mucous membranes. These mistakes happen because labels aren’t clear, or people don’t read them. The Agency for Healthcare Research and Quality found that 16% of medication errors involve the wrong route. Always check the instructions: “Oral,” “Topical,” “Inhalation,” “Subcutaneous.” If you’re unsure, ask. If your doctor says “apply to skin,” don’t assume it’s safe to swallow. If your inhaler says “for oral use only,” don’t spray it into your nose. And never mix medications-like putting liquid antibiotics into a nebulizer unless it’s specifically designed for that.Rule 5: Confirm the Right Patient
This rule isn’t just for hospitals. At home, it’s easy to mix up pills, especially in households with multiple people taking similar medications. A husband might grab his wife’s blood thinner, thinking it’s his daily aspirin. A child might take a parent’s painkiller, mistaking it for candy. Even in pharmacies, mix-ups happen. Always verify your name and date of birth when picking up prescriptions. Keep your medications in their original bottles with labels intact. Never transfer pills to unmarked containers unless you’ve labeled them clearly with the drug name, dose, and purpose. If you’re caring for someone else, use color-coded pill boxes with the person’s name printed on each compartment. And never share prescriptions-even if you think your symptoms are the same.What You’re Not Being Told
The Five Rights-right patient, drug, dose, route, time-are the foundation. But safety doesn’t stop there. You also need to know the right reason for taking the drug, the right response to expect, and the right way to document any side effects. Many people don’t realize that medications can interact with foods, supplements, or even other prescriptions. For example, grapefruit juice can make cholesterol meds like atorvastatin dangerously strong. St. John’s Wort can cancel out birth control pills. And if you’re on blood thinners, suddenly eating more kale or spinach can mess with your INR levels. Always ask: “Could this interact with anything else I’m taking?”
Tools That Actually Help
You don’t need fancy tech to stay safe. But simple tools make a big difference:- Use a pill organizer with days and times labeled
- Download a free app like Medisafe or MyTherapy to set reminders
- Keep a written list of every medication, including doses and why you take them
- Bring all your meds (in their original bottles) to every doctor visit-this is called a “brown bag review”
- Ask your pharmacist to review your list every 3 months
What to Do If Something Feels Wrong
If you feel dizzy, nauseous, confused, or notice unusual bruising or bleeding after starting a new med, don’t wait. Call your doctor or pharmacist immediately. Don’t assume it’s “just side effects.” Some side effects are normal. Others are warning signs. If you’re ever unsure, err on the side of caution. Better to check and find nothing than to ignore a red flag.Final Thought: Safety Is a Habit, Not a One-Time Task
Medication safety isn’t something you do once when you get your prescription. It’s a daily practice. It’s checking labels every time you open a bottle. It’s asking questions even when you feel silly. It’s keeping your list updated. It’s knowing that your body changes-and so might your needs. The goal isn’t perfection. It’s awareness. The more you know, the less likely you are to become one of the 1.3 million people who end up in the ER because of a preventable mistake.What should I do if I miss a dose of my medication?
Don’t double up unless your doctor says so. Check the label or call your pharmacist. For most drugs, if you remember within a few hours of the missed dose, take it right away. If it’s close to the next scheduled dose, skip the missed one and go back to your regular schedule. For high-risk meds like blood thinners or insulin, always call your provider-wrong timing can be dangerous.
Can I crush my pills if I have trouble swallowing them?
Only if the label or your pharmacist says it’s safe. Many pills-especially extended-release, enteric-coated, or capsule forms-are designed to release slowly. Crushing them can cause too much medicine to enter your system at once. For example, crushing a long-acting opioid can lead to overdose. Always ask before crushing or opening capsules.
Why do some medications need to be taken with food and others without?
Food can affect how your body absorbs medicine. Some drugs, like antibiotics (e.g., amoxicillin), work better with food to reduce stomach upset. Others, like thyroid meds (levothyroxine), need an empty stomach because food blocks absorption. Fatty meals can make certain cholesterol drugs more effective. Always follow the instructions on the label or ask your pharmacist why timing matters.
Are over-the-counter drugs really safe to take with my prescriptions?
Not always. Common OTC drugs like ibuprofen, antacids, or cold medicines can interact badly with prescriptions. Ibuprofen can increase bleeding risk if you’re on warfarin. Antacids can block absorption of antibiotics or thyroid meds. Even vitamin supplements like vitamin K can interfere with blood thinners. Always tell your doctor and pharmacist everything you’re taking-even herbs and supplements.
How do I know if a medication has expired and is still safe to use?
Check the expiration date on the bottle. After that date, the drug may lose potency or break down into harmful substances. Some meds, like insulin or liquid antibiotics, become unsafe quickly after expiration. Solid pills might still work for a short time past the date, but you can’t rely on it. If it looks discolored, smells odd, or has changed texture, throw it out. Never take expired heart meds, antibiotics, or epinephrine.
What should I do with old or unused medications?
Don’t flush them or toss them in the trash. Many pharmacies have drug take-back programs. If none are available, mix pills with coffee grounds or cat litter in a sealed bag before throwing them away. This prevents accidental ingestion by kids or pets. Remove personal info from bottles before recycling them. Never keep old meds “just in case”-they can expire, get mixed up, or be taken by someone else.




Okay but let’s be real - most people don’t even know what ‘generic name’ means. I had a friend take two different bottles of ‘blood pressure pills’ for months because one said ‘amlodipine’ and the other said ‘Norvasc.’ Same drug. She thought she was doubling up. Ended up in the ER with a heart rate of 38.
Pharmacists aren’t paid to explain this stuff. Doctors are rushed. So you’re left holding a pill bottle like it’s a magic rune. And yeah - color and shape change all the time. I’ve had my metformin look like a tiny blue dinosaur one month and a white oval the next. No warning. Just… different.
Rule 1 should be: ‘Always Google the generic name + your brand name.’ And screenshot it. Save it. Treat it like a passport.
Five rules? That’s it? You’re telling me the entire U.S. healthcare system’s medication disaster can be fixed by telling people to read labels?
What about the 60-year-old on Medicare who gets 14 prescriptions from 7 different doctors and can’t afford to see a pharmacist? Or the single mom who’s working two jobs and forgets which pill is for her thyroid and which is for her anxiety because they’re both white and round?
This isn’t about ‘awareness.’ It’s about a system that treats patients like disposable code.
USA still the best at this. Other countries? They give you a pamphlet in 12 languages and hope you don’t die. Here? We got apps, pill organizers, brown bag reviews - and if you still can’t figure out ‘take with food’ then maybe you shouldn’t be allowed to own a phone.
Also - why are we letting Indians and Nigerians comment on this? You guys don’t even have pharmacies with AC. My cousin in Delhi still uses a spoon to measure insulin. I’m not being racist - I’m being realistic.
HAHAHAHA! So you think ‘read the label’ is the solution?! You’re living in a 1990s sitcom! In India, we have pharmacies where the guy behind the counter just hands you whatever he thinks you need - no script, no questions, just ‘beta, yeh lo, do din mein theek ho jayega!’
And then people wonder why we have 40% antibiotic resistance?!
Stop pretending this is a ‘personal responsibility’ issue. It’s a cultural, economic, and corporate failure. Your ‘five rules’ are like telling someone to ‘not get hit by a car’ while giving them a broken bicycle and a highway with no lights.
It is profoundly irresponsible to frame medication safety as a matter of individual diligence. The onus is not on the patient to decode pharmaceutical obfuscation. The system - the pharmaceutical corporations, the insurance gatekeepers, the fragmented care models - must be held accountable.
One cannot reasonably expect a person with limited literacy, cognitive load, or economic precarity to navigate a labyrinth designed to maximize profit, not safety.
This article is not informative - it is a moral evasion.
just take your pills. dont overthink it. your body knows what to do.
if you feel weird? stop. call someone.
that’s it. really.
Oh my GOD. I just realized my neighbor takes the same pills as me - same color, same shape - and I’ve been taking hers for weeks because I thought they were mine 😭😭😭
Now I’m scared to even open my cabinet. What if I’ve been taking someone else’s antidepressants?! What if I’m not even me anymore?!
Also - did you know that Big Pharma puts secret mind-control chemicals in blood pressure meds? I read it on a blog. They’re testing on us. I’m not paranoid. I’m PREPARED. 💀
I love how this post says ‘ask questions’ but doesn’t mention that half the time, doctors roll their eyes when you do.
I asked my cardiologist why my new pill was blue instead of white. He said, ‘It’s the same thing.’ I said, ‘But last month it was white.’ He said, ‘You’re overthinking.’
Then I Googled it. Turns out the new version has a different filler that causes my ankles to swell.
So yeah - ask. But also keep receipts. And screenshots. And maybe a lawyer.
Let me guess - this was written by someone who works for a pharmaceutical company.
‘Know what you’re taking’? Sure. But what if your meds are being changed without your knowledge? What if your insurance switches your brand to a cheaper generic that’s not bioequivalent? What if your doctor is being paid by the manufacturer to prescribe certain drugs?
You think the label tells you the truth? The FDA approves drugs based on 6-month trials. Real-world effects? They don’t track it.
And don’t get me started on the fact that 80% of ‘essential’ meds are made in China. You have no idea what’s actually in that pill.
Hey - I’ve been a nurse for 22 years. I’ve seen people die because they didn’t know the difference between ‘take with food’ and ‘take on empty stomach.’
But I’ve also seen people thrive because they kept a little notebook. Wrote down the date, the pill, how they felt. Took photos of their bottles.
You don’t need to be a genius. You just need to be consistent.
Start small. One pill. One question. One pharmacist chat. You got this.
Rule 1: Know what you’re taking - yet most people don’t even know the difference between a vitamin and a medication.
And yet - you see people taking 12 supplements, 5 prescriptions, and a ‘natural energy booster’ from Amazon - and then wonder why they’re dizzy.
It’s not rocket science. But it requires discipline. And discipline? That’s rare.
Most people want a magic pill. But safety? It’s not a pill. It’s a practice. And most won’t do the work. So they end up in the ER. And then they blame the system.
Wake up. Your health is your responsibility. Not the pharmacist’s. Not the doctor’s. Yours.