How to Share Over-the-Counter and Supplement Use Accurately with Your Provider
Every year, millions of people take over-the-counter medicines and dietary supplements without telling their doctors. They think it’s harmless. Maybe they believe supplements are "natural," so they don’t count. Or maybe their provider never asked. But here’s the truth: OTC medications and supplements can be just as dangerous as prescription drugs when they interact with them.
In 2022, the FDA logged over 1,000 adverse events tied to supplements - including 52 deaths. Many of these could have been avoided if patients had shared exactly what they were taking. The problem isn’t the supplements themselves. It’s the silence.
Why Your Provider Needs to Know What You’re Taking
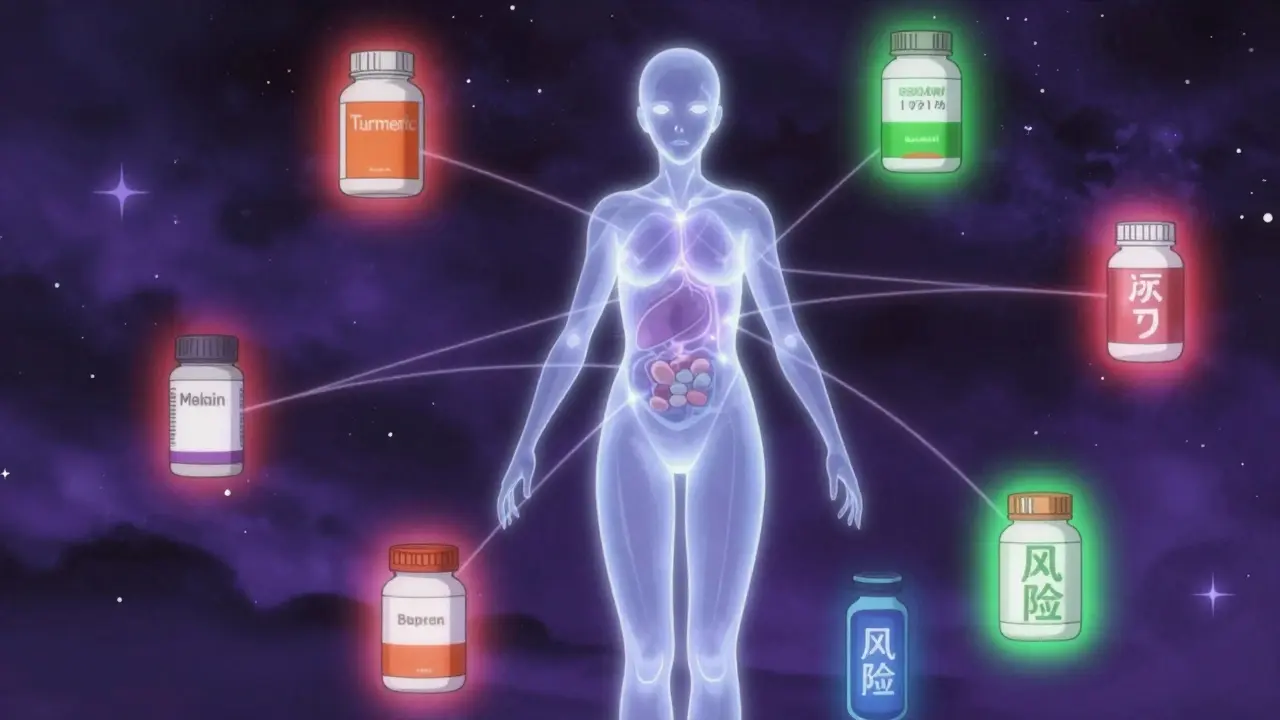
Think of your body like a complex machine. Prescription drugs, OTC painkillers, vitamins, herbal extracts - they all send signals. Some are helpful. Some clash. When you take fish oil with blood thinners like warfarin, it can increase bleeding risk. St. John’s Wort can make birth control, antidepressants, or even chemotherapy less effective. Kava and comfrey, often sold as "natural" remedies, have caused liver failure when mixed with certain medications.
The FDA doesn’t approve supplements before they hit shelves. Unlike prescription drugs, they don’t need safety testing or clinical trials first. Manufacturers only need to prove they’re not harmful after the fact. That means you’re the first line of defense. If you don’t tell your provider, they can’t protect you.
Studies show 37.9% of U.S. adults take supplements. But only 36% tell their doctors. Meanwhile, 23% of hospital patients experience potential drug-supplement interactions - and nearly 8% of those are severe. That’s not a small risk. That’s a pattern.
What Counts as a Supplement? (And Why You’re Probably Missing Some)
Most people think supplements are just multivitamins or fish oil. But the list is longer than you think:
- Vitamins (D, B12, C)
- Minerals (magnesium, zinc, calcium)
- Herbs (echinacea, turmeric, ginkgo)
- Probiotics
- Protein powders
- Weight loss pills
- Energy boosters
- Sleep aids (melatonin, valerian root)
- Joint support (glucosamine, chondroitin)
And don’t forget OTC medicines. Tylenol, ibuprofen, antacids, allergy pills, cough syrups - these are drugs too. Many people don’t realize that taking Advil every day for back pain counts as medication use. Same with daily antacids or nighttime sleep aids.
Here’s the kicker: 64% of people don’t consider vitamins and minerals as "supplements" that need to be disclosed. That’s a dangerous assumption. A daily 1,000 mg vitamin D pill isn’t just a "healthy habit." It’s a pharmacologically active substance that can affect calcium levels, kidney function, and interact with steroids or cholesterol drugs.
The Right Way to Track Your Medications and Supplements
Memory fails. Labels get lost. Bottles get mixed up. That’s why you need a written record - not just a mental list.
The National Institutes of Health (NIH) created a simple, free tool called the My Dietary Supplement and Medicine Record. Use it. Fill it out before every appointment. Include:
- Exact product name - not "vitamin C" but "Nature Made Vitamin C 500 mg tablets"
- Dosage - "500 mg twice daily" not just "vitamin C"
- Frequency - "every morning," "as needed for headaches," "three times a week"
- Purpose - "for bone health," "to reduce inflammation," "for better sleep"
Write down every prescription, OTC medicine, and supplement. Even the ones you only take occasionally. Even the ones you got from a friend or bought online.
Research shows patients who use a written list reduce documentation errors by 64% compared to those who just talk. That’s not a small improvement. That’s life-saving.
What to Say - and How to Say It
Providers don’t always ask. In fact, 52.7% of people who don’t disclose supplements say their provider never brought it up. Don’t wait for them to ask. Take control.
At your next visit, say this:
"I want to make sure you know everything I’m taking - not just my prescriptions, but also my vitamins, supplements, and OTC medicines. Here’s my list. Can we go through it together?"
Be specific. Don’t say, "I take some herbs." Say, "I take turmeric capsules, 1,500 mg daily, for my arthritis." Don’t say, "I use melatonin." Say, "I take 3 mg of melatonin every night at 10 p.m. to help me sleep."
Pharmacists are especially good at catching interactions. In one study, pharmacists found 3.2 times more supplement-drug risks than doctors during medication reviews. If you see a pharmacist for a refill or consultation, hand them your list too.
What Happens When You Don’t Tell
The consequences aren’t theoretical. They’re documented.
A 45-year-old woman died in 2019 from liver failure after taking kava supplements while on antipsychotic medication. Her doctors never knew she was using it. A 68-year-old woman avoided life-threatening bleeding because her provider spotted her daily 1,000 mg fish oil dose - a known blood thinner - and adjusted her warfarin. A man on statins developed severe muscle pain after starting CoQ10, thinking it would help. His provider didn’t know about it until he was hospitalized.
And it’s not just rare cases. In 2022, the FDA received over 1,000 reports of adverse events from supplements. Green tea extract combined with acetaminophen caused liver failure in multiple cases. Iron supplements taken with thyroid meds blocked absorption. Garlic supplements boosted the effect of blood thinners to dangerous levels.
These aren’t accidents. They’re communication failures.
How Technology Is Helping - But Still Falling Short
Electronic health records (EHRs) are supposed to help. But only 31% of primary care systems have dedicated fields for supplement documentation. Most still lump everything under "medications," making it easy to miss.
Some big systems are catching up. Epic Systems added supplement tracking in 2020. By 2024, they’ll roll out AI-powered screening that checks 14,700 supplement products against prescription databases. That’s progress.
But tech won’t fix the problem if providers don’t ask. And patients don’t speak up. The American Medical Informatics Association found only 34% of clinicians routinely use structured supplement screening tools. At Mayo Clinic, where mandatory screening was added in 2020, supplement-related adverse events dropped by 37%. That’s proof it works.
Don’t wait for your provider to upgrade their system. Do your part now.
Common Myths That Keep People Silent
Here are the top three reasons people don’t tell their provider - and why they’re wrong:
- "It’s just a vitamin." - Wrong. Vitamin D, K, and A can be toxic in high doses. Iron can damage your liver. B6 can cause nerve damage.
- "My doctor doesn’t care about supplements." - Maybe they didn’t ask. But 4.7 out of 5 patient satisfaction ratings go to providers who do ask. Your provider wants to keep you safe.
- "I didn’t think it was important." - 63% of people who had side effects from supplements didn’t report them for this reason. But 28% of consumers experience interactions between supplements and medications. That’s not rare. That’s common.
Supplements aren’t harmless. They’re unregulated. And that’s why your honesty matters more than ever.
What to Do Today
You don’t need to wait for your next appointment. Start now:
- Look in your medicine cabinet. Pull out every bottle - prescriptions, OTC, vitamins, herbs, powders.
- Write down the exact name, dose, frequency, and reason for each one.
- Use the NIH form or just a piece of paper. Be specific.
- Bring it to your next visit - even if it’s a quick checkup.
- Ask: "Can we review this together? I want to make sure nothing here is risky."
It takes 10 minutes. But it could save your life.
And if your provider doesn’t ask? Ask them. Say: "I’ve been reading about supplement interactions. I want to make sure I’m safe. Can we go over everything I’m taking?"
You’re not being difficult. You’re being smart. And you’re doing exactly what the FDA, NIH, and the American Medical Association all recommend.


Just took my fish oil and turmeric this morning. Never thought about how that might mess with my blood pressure med. Thanks for the wake-up call.
Oh great, now I’m supposed to keep a spreadsheet of every pill I swallow? Next they’ll want me to log my breathing patterns and dream cycles. This is how control starts.
I’m a nurse in rural Ohio. Every week, someone comes in with liver enzymes through the roof because they took ‘natural’ liver cleanse tea with their statin. No one ever thinks it’s a problem until it’s an emergency. Please, just write it down. It takes 5 minutes.
Big Pharma doesn’t want you to know supplements work better than their overpriced pills. They’re scared. That’s why they push this fear crap. You’re being manipulated.
Wow. So the real problem isn’t supplements-it’s that doctors don’t ask like they’re trying to solve a crossword puzzle blindfolded. Also, melatonin at 3mg? That’s basically a sedative. You’re not ‘helping sleep,’ you’re chemically knocking yourself out.
The FDA logged 1,000 adverse events? That’s nothing. They ignore 90% of reports. And who’s funding those studies? Big supplement companies? Big pharma? You think they’d let the truth out? Wake up.
I’ve been taking magnesium for migraines for years. My doctor never asked. Last month, I mentioned it offhand-turns out it was interacting with my heart med. We adjusted it. No drama. Just honesty. Thanks for reminding me to be that person.
Just made a list. Took 8 minutes. Included my gummy vitamins, my neighbor’s ‘immune booster’ powder, and the cough syrup I take when I’m sick. I’m bringing it to my appointment Friday. Simple. Smart.
It is imperative to underscore that the pharmacokinetic and pharmacodynamic interactions between nutraceuticals and pharmaceuticals constitute a clinically significant public health concern. The absence of standardized nomenclature and regulatory oversight exacerbates diagnostic ambiguity and increases iatrogenic risk.
My grandma took garlic pills for 20 years. Never had a problem. My uncle took 12 prescriptions and died of a heart attack. So maybe the real issue isn’t supplements-it’s doctors who think they know everything.
This is a textbook example of the erosion of personal responsibility. If you can’t manage your own health, why should your doctor be burdened with your poor choices? The solution isn’t more forms-it’s more discipline.
In Nigeria, we call this ‘talking to the medicine.’ Our elders always said: ‘If you take two things, tell the healer.’ It’s not new. It’s wisdom. I’m glad someone finally wrote it in English so it doesn’t get lost.
i mean… if supplements are so dangerous… why do we have them at all? why not just ban them? if they’re so risky… then why is the FDA only tracking 1000 cases? sounds like they’re not really trying… or maybe i’m just overthinking
As a public health advocate, I commend this article for its clarity and actionable steps. In India, where polypharmacy is rampant and supplement use is rising rapidly, structured patient education must be integrated into primary care. This is not just advice-it is a public health imperative.
My cousin took 10 different supplements and ended up in the ER. His doctor said, ‘You didn’t tell me you were taking that green powder from the guy at the gas station?’ That’s not a mistake. That’s a horror story. And now he’s on dialysis. Don’t be that guy.