Gut Health and Skin Conditions: What the Latest Research Reveals
Gut-Skin Connection Assessment Tool
Your Gut-Skin Assessment Results
Your Score:
Acne
Eczema
Psoriasis
Recommendations Based on Your Profile
Ever wondered why a flare‑up on your face sometimes seems to follow a bad pizza night? The answer may lie deeper than the surface - in the bustling community of microbes living in your gut. Scientists are now piecing together a clear picture of how gut health influences skin conditions ranging from stubborn acne to itchy eczema.
Key Takeaways
- The gut‑skin axis is a two‑way street: gut microbes affect skin inflammation, and skin stress can alter gut balance.
- High‑quality studies link dysbiosis (an unhealthy gut microbiome) with acne, atopic dermatitis, and psoriasis.
- Targeted diet changes, probiotic supplements, and lifestyle habits can improve both gut and skin health.
- Not all probiotics work the same; strain specificity matters.
- If skin issues persist, a dermatologist or gastroenterologist can help rule out underlying conditions.
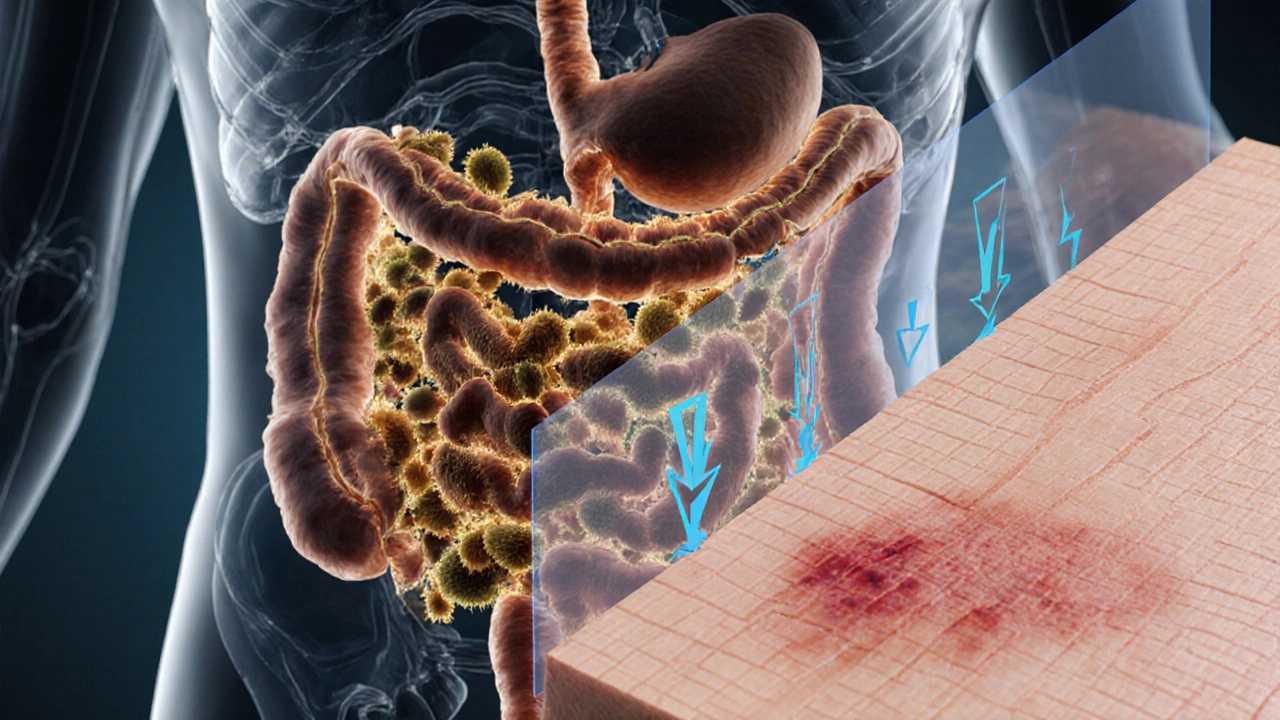
Understanding the Gut‑Skin Axis
At the core of the connection is the gut microbiome the trillions of bacteria, fungi and viruses that live in the digestive tract and help digest food, train the immune system, and produce signaling molecules. When the microbiome is balanced, it supports a strong skin barrier and modulates inflammation.
The skin itself has its own ecosystem, often called the skin barrier the outermost layer of the epidermis that keeps moisture in and harmful agents out. Disruption of the barrier leads to dryness, redness, and creates a foothold for pathogens.
Inflammation is the biochemical bridge. A leaky gut (also known as leaky gut syndrome a condition where intestinal tight junctions become more permeable, allowing larger particles to enter the bloodstream) permits endotoxins and undigested food particles to travel to the bloodstream, triggering systemic inflammation that shows up as skin flare‑ups.

What the Latest Research Says
Researchers have used three main approaches to map the gut‑skin relationship: human cohort studies, animal models, and intervention trials.
- Human cohort studies have consistently found that people with severe acne or eczema often have reduced microbial diversity and lower levels of beneficial bacteria such as Lactobacillus and Bifidobacterium. A 2023 Finnish study of 1,200 adolescents reported a 30% higher odds of moderate‑to‑severe acne in participants whose gut diversity fell in the lowest quartile.
- Animal models allow scientists to manipulate gut microbes directly. Mice given a high‑fat, low‑fiber diet develop both gut dysbiosis and increased skin inflammation, an effect that disappears when the diet is switched back to high‑fiber.
- Intervention trials give the most actionable data. A double‑blind, placebo‑controlled trial in 2022 gave 150 adults with mild‑to‑moderate psoriasis a 12‑week course of probiotic live microorganisms that, when administered in adequate amounts, confer a health benefit on the host containing Streptococcus thermophilus and Lactobacillus plantarum. Participants saw a 20% reduction in PASI scores (a standard psoriasis severity index) compared to a 5% reduction in the placebo group.
Collectively, the evidence points to a moderate‑to‑strong link between gut composition and skin health, especially for inflammatory conditions.
Skin Conditions Most Affected by Gut Health
Not every skin issue responds to gut‑focused interventions. Below is a snapshot of the three conditions with the strongest research backing.
| Condition | Typical Gut Signature | Research Consensus (2020‑2025) |
|---|---|---|
| Acne | Low short‑chain fatty acids metabolites like butyrate that reduce inflammation, reduced Cutibacterium diversity | Moderate‑to‑strong (multiple RCTs show benefit of probiotics and low‑glycemic diets) |
| Eczema (Atopic Dermatitis) | Decreased Bifidobacterium, increased Clostridium difficile colonization | Strong (prenatal probiotic supplementation lowers infant eczema risk by ~25%) |
| Psoriasis | Higher Firmicutes‑to‑Bacteroidetes ratio, elevated inflammatory cytokines (IL‑17, TNF‑α) | Moderate (probiotic and high‑fiber interventions show modest PASI improvements) |
Practical Steps to Boost Gut Health for Clearer Skin
Translating research into daily habits doesn’t have to be overwhelming. Focus on three pillars: diet, targeted microbes, and lifestyle.
- Fiber‑rich foods: Aim for 25‑30g of soluble fiber per day. Oats, legumes, berries, and especially chicory root feed beneficial bacteria that produce short‑chain fatty acids, which calm skin inflammation.
- Fermented foods: Include a serving of kefir, kimchi, sauerkraut, or unsweetened yogurt daily. These provide live cultures that can help restore balance.
- Probiotic supplements: Choose strains that have shown skin benefits. For acne, Lactobacillus rhamnosus GG and Bifidobacterium breve are frequently cited. For eczema, Lactobacillus reuteri and Bifidobacterium lactis are top picks. Take them with a meal to improve survival through stomach acid.
- Prebiotic boosters: In addition to fiber, consider inulin a plant‑derived prebiotic fiber found in garlic, onions, and Jerusalem artichoke or galactooligosaccharides (GOS) as a supplement.
- Limit gut irritants: Reduce ultra‑processed foods, excessive alcohol, and high‑sugar snacks. These promote dysbiosis and increase gut permeability.
- Stress management: Chronic stress elevates cortisol, which can weaken the gut barrier. Simple practices like 10‑minute breathing exercises, short walks, or yoga can keep the microbiome happy.
For many people, noticeable skin improvement appears after 4‑8weeks of consistent changes. Keep a simple journal of diet, supplements, and skin flare‑ups to spot patterns.
When to Seek Professional Help
If you’ve tried the above steps for three months and your skin hasn’t budged, it’s time to bring in a specialist. Dermatologists can rule out hormonal or medication‑related causes, while gastroenterologists can test for small‑intestine bacterial overgrowth (SIBO) or celiac disease, both of which can masquerade as skin problems.
Blood tests for inflammatory markers (CRP, IL‑6) and stool analyses for microbiome profiling are becoming more accessible and can guide personalized probiotic or dietary prescriptions.
Frequently Asked Questions
Can gut health really clear up acne?
Yes. Multiple randomized trials show that specific probiotic strains-especially Lactobacillus rhamnosus GG and Bifidobacterium breve-reduce inflammatory lesions by 15‑30% when taken for 8‑12 weeks alongside a low‑glycemic diet.
Is a gluten‑free diet necessary for skin health?
Only if you have celiac disease or a proven gluten sensitivity. For most people without these conditions, eliminating gluten doesn’t provide added skin benefit and may reduce fiber intake.
How long does it take to see results from probiotics?
Skin improvements typically appear after 4-8 weeks of daily use. Consistency matters; stopping the supplement often leads to a return of symptoms within a month.
Are there any risks to taking probiotic supplements?
For healthy adults, probiotics are generally safe. People with severely compromised immune systems should consult a doctor first, as rare cases of bloodstream infection have been reported.
What foods boost short‑chain fatty acid production?
Foods rich in soluble fiber-like oats, bananas, apples, legumes, and especially chicory root-fuel bacteria that produce butyrate and propionate, both of which have anti‑inflammatory effects on the skin.

Interesting summary of the gut‑skin axis; the evidence linking microbial diversity to acne and eczema is becoming pretty solid.
I totally get how overwhelming all this data can feel 😊. Your breakdown of fiber, fermented foods and stress really hits the nail on the head, and it’s great that you included actionable steps. It’s amazing how short‑chain fatty acids act like tiny diplomats, calming inflammation both in the gut and on the skin. Keep spreading this knowledge – the more people that understand the connection, the better for everyone’s complexion.
Great tips, thanks!
When I first read about the gut‑skin axis I felt like a scientist discovering a hidden continent beneath the surface of our bodies.
The gut, teeming with trillions of microbes, is not merely a passive digestion tank but a bustling metropolis that whispers to our skin.
Each fiber molecule we ingest fuels beneficial bacteria, which in turn generate short‑chain fatty acids that act as peacekeepers against inflammation.
Conversely, a diet heavy in processed sugars and saturated fats is akin to sending a marauding army that destabilizes the microbial equilibrium.
The resulting dysbiosis can open the doors to leaky gut, allowing endotoxins to flood the bloodstream and incite the angry immune response we recognize as acne or eczema.
Clinical trials from Finland to Finland? Actually across Europe consistently show that probiotic strains like Lactobacillus rhamnosus GG reduce lesion counts by up to thirty percent.
What astonishes me further is the role of stress, the silent puppeteer that pulls at the gut barrier, amplifying cortisol‑driven permeability.
Studies reveal that a simple ten‑minute mindfulness practice can lower cortisol, improve microbial diversity, and, after weeks, visibly calm the skin.
Even more compelling is the emerging evidence that prebiotic fibers such as inulin not only feed good bacteria but also directly modulate immune signaling pathways.
If you think about the evolutionary partnership between humans and microbes, it becomes clear that we are not just hosts but co‑creators of our own dermal destiny.
Therefore, ignoring gut health while obsessing over topical creams is like patching a leak without fixing the broken pipe.
The practical takeaway is simple: prioritize whole foods, fermented delights, and consistent probiotic supplementation.
And, crucially, give your body time-most skin improvements reveal themselves after four to eight weeks of steadfast commitment.
Remember, the gut‑skin axis is a two‑way street; a healthier gut paves the way for clearer skin, and clearer skin can boost confidence, closing the feedback loop.
So, let us raise our kefir glasses and toast to a future where the microbiome is the unsung hero of radiance.
Honestly, after reading the whole piece I feel it’s a bit overhyped, even though there’s some truth to the fiber‑probiotic link. The article throws a lot of studies at you without really saying which ones matter most. It’s like trying to drink from a fire hose while also trying to juggle orange slices. I get that gut health matters, but you could have summarized the key points in half the space. Also, the recommendations feel generic – “eat more veggies, take probiotics” is something we’ve heard a million times. Some readers might appreciate the detailed tables, yet they distract from practical advice. In short, good intentions, but execution feels lazy. Maybe next time tighten the focus.
This is definetly the kind of nonsense that makes me roll my eyes. The author is pushing some fad diet without real proof and it’s a waste of time. If you take all those probiotic hype you’ll just waste money and get no results. Stop falling for marketing gimmicks and read real science, not whatever they put together here. It’s infuriating how people still believe this junk. Get a grip and stop spreading it.
What a spectacular display of half‑baked wellness talk! The article tries to sound scholarly while spouting the same tired claims you see on every health blog. It’s almost comical how it glosses over the complexities of the microbiome and pretends a single supplement can fix everything. If only readers demanded rigor instead of glossy recipes, maybe we’d see real progress.
There are a few practical steps you can start with: first, aim for at least 25 grams of soluble fiber daily – think oats, legumes, and berries. Second, incorporate a serving of fermented foods like kefir or kimchi each day to introduce live cultures. Third, choose a probiotic that lists strain numbers, such as Lactobacillus rhamnosus GG (ATCC 53103) and Bifidobacterium breve (DSM 20213). Finally, track your skin changes in a simple journal to see what works for you.
Thx for the clear action plan it really helps i will try to add more fiber and kefir soon the journal idea is great for spotting patterns .
While the article presents a neat narrative, one must consider who benefits from this probiotic push – the supplement industry. There’s a subtle agenda to monetize our gut, turning every microbiome nuance into a product. Independent research often gets buried behind paywalls while corporate‑funded trials get glossy headlines. Question the source and you’ll see the story isn’t as simple as “eat yogurt, get clear skin”.
Exactly, they’re using our desire for clear skin as a Trojan horse to get us to swallow pills they claim are “science”. The real truth is that many of these strains are engineered, and the long‑term effects are unknown. Don’t be fooled by slick marketing – the gut‑skin axis is complex and can’t be reduced to a bottle of capsules.
A balanced approach is best – incorporate whole foods, be mindful of stress, and view supplements as an adjunct, not a cure‑all.
Oh, come on! You’re telling us that a spoonful of fermented cabbage can outshine a dermatologist’s prescription? That’s a rainbow of hyperbole, dripping with over‑optimism. While gut health matters, let’s not pretend it’s a miracle potion that erases every blemish.
Actually, the evidence is still mixed; some studies find a link, others see no effect, so it’s premature to claim a definitive gut‑skin cure.
🔥💥 Absolutely! The gut‑skin saga is a rollercoaster of hype and hope, and we’re all just trying to catch the next breakthrough! 🌟🤯
I appreciate the thoroughness of the guide it covers diet probiotics and lifestyle changes all in one place nice work