Generic Price Transparency: Tools to Find the Best Price for Prescription Medications

When you need a generic medication, you expect it to be cheap. But sometimes, the same pill costs $4 at one pharmacy and $45 at another-right down the street. Why? Because drug pricing in the U.S. isn’t simple. It’s layered with rebates, contracts, and hidden discounts that even doctors don’t always understand. The good news? You don’t have to guess anymore. Tools exist to show you the real price before you pay.
Why Generic Drug Prices Vary So Much
Generic drugs are supposed to be affordable copies of brand-name medicines. But the price you see on the shelf isn’t the whole story. The list price, called the Wholesale Acquisition Cost (WAC), is what manufacturers charge pharmacies. But that’s not what pharmacies actually pay. Pharmacy Benefit Managers (PBMs)-middlemen between insurers and pharmacies-negotiate secret rebates with drug makers. Those rebates lower the net price, but they’re never shown to you at the counter. Meanwhile, pharmacies set their own retail prices based on what they think you’ll pay. Some use Maximum Allowable Cost (MAC) lists to cap how much they’ll pay for generics. Others mark up prices to cover overhead. That’s why two identical prescriptions can cost wildly different amounts. A 30-day supply of metformin might be $3 at Walmart, $18 at a local pharmacy, and $22 at a chain store-even with the same insurance.Real-Time Benefit Tools: What Doctors Use
If you’ve ever had your doctor pause mid-prescription to check your phone, they’re probably using a Real-Time Benefit Tool (RTBT). These are systems built into electronic health records like Epic and Cerner that pull your insurance details and show you exactly how much your copay will be before the prescription is sent. Platforms like CoverMyMeds and Surescripts connect directly to your insurer’s system. They show you:- Your exact out-of-pocket cost for the prescribed drug
- Lower-cost alternatives on your plan’s formulary
- Eligibility for patient assistance programs
GoodRx and Other Consumer Apps
You don’t need a doctor’s office to find a better price. Apps like GoodRx, SingleCare, and RxSaver let you compare cash prices at nearby pharmacies. They don’t use your insurance-they show you what you’d pay if you paid out of pocket. GoodRx, used by 43% of U.S. pharmacies, is the most popular. It works like a coupon: you enter your drug, zip code, and dosage, and it lists prices at CVS, Walgreens, Kroger, and independent pharmacies. Sometimes, the cash price is lower than your insurance copay. But here’s the catch: the prices you see aren’t always guaranteed. A user on Trustpilot reported going to a pharmacy where the app showed $4 for lisinopril-but the pharmacist said their system said $15. That’s because the app pulls from a network of contracted pharmacies, and not all locations update in real time. Some pharmacies honor the price; others don’t. These apps are best for people without insurance, those with high-deductible plans, or those buying medications not covered by their plan. They’re also great for comparing prices before you walk in.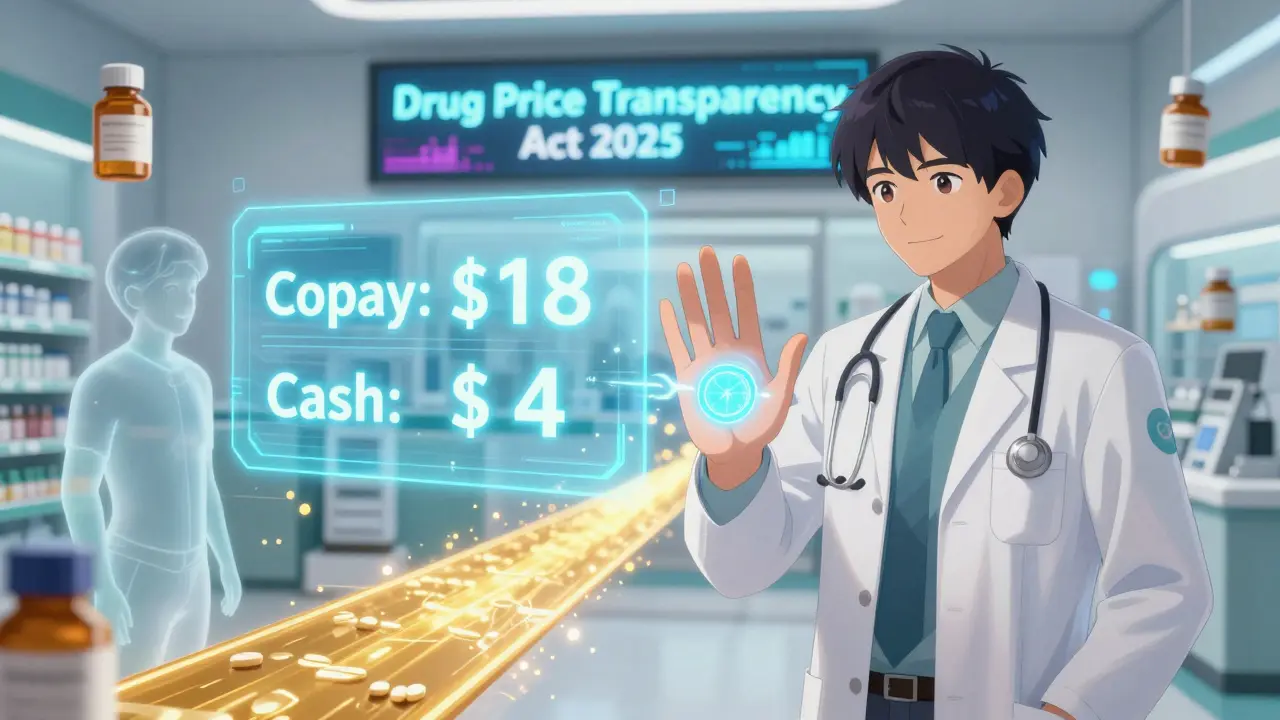
State Laws and Public Portals
Some states are stepping in where federal rules fall short. As of April 2025, 23 states have passed laws requiring drug manufacturers to report price hikes. Twelve have created Prescription Drug Affordability Boards (PDABs) that review whether a drug’s cost is reasonable. In Minnesota, a patient used the state’s transparency portal to find a 92% price difference for the same generic drug between two pharmacies just five miles apart. She saved $287 a year by switching. California requires drugmakers to report any price increase over 16% in two years. New York and Washington have similar rules. These laws don’t cap prices, but they force transparency-and that pressure often leads to lower costs. You can search your state’s health department website for a drug price lookup tool. Many states list average prices for common generics, and some let you compare pharmacies directly.What You Can Do Right Now
You don’t need to wait for a law or a doctor’s visit to save money. Here’s what works today:- Ask your pharmacist for the cash price. Always. Even if you have insurance, the cash price might be lower.
- Use GoodRx or SingleCare. Compare prices before you leave home.
- Check RxAssist.org. This nonprofit database helps you find free or discounted drugs from manufacturer programs. Over 1.2 million people used it in 2024.
- Ask your doctor for alternatives. If you’re prescribed a brand-name drug, ask: “Is there a generic? Is there a cheaper generic?”
- Buy in bulk. Many pharmacies offer 90-day supplies at the same price as 30-day ones.

The Big Limitation: Net Prices Are Still Hidden
The biggest problem with all these tools? They don’t show you the net price-what the insurer and PBM actually paid after rebates. That number is secret. So even if you find a $5 generic, the real cost to the system might be $1.50. But you never see that. That’s why some experts say transparency alone won’t fix drug pricing. If the rebate system stays hidden, manufacturers have no incentive to lower list prices. In fact, they might raise them to create bigger rebates-and bigger profits. Still, for you, the patient, knowing the cash price or your copay is enough to make smarter choices. You don’t need to fix the whole system. You just need to know what you’re paying.What’s Coming in 2025 and Beyond
The Drug-price Transparency for Consumers Act (S.229), introduced in January 2025, would force drug companies to show the wholesale cost in TV and print ads. If passed, you’d see something like: “$120 for a 30-day supply of metformin.” That’s a big step toward clarity. The Centers for Medicare & Medicaid Services (CMS) is also expected to release new rules by the end of 2025 requiring insurers to report total drug spending after rebates. That won’t change your bill tomorrow-but it could pressure PBMs to be more honest about pricing. For now, the tools you have are enough. They’re not perfect. But they’re better than guessing.Why is my generic drug so expensive even though it’s not brand-name?
Generic drugs are cheaper than brand names, but prices still vary because pharmacies set their own retail prices, and Pharmacy Benefit Managers (PBMs) negotiate secret rebates with drug makers. What you pay at the counter is often unrelated to what the pharmacy actually paid. Some pharmacies use Maximum Allowable Cost (MAC) lists to cap prices, while others mark them up. Always ask for the cash price-it might be lower than your insurance copay.
Can I use GoodRx with my insurance?
No, GoodRx doesn’t work with insurance. It shows you the cash price at pharmacies, which can sometimes be cheaper than your insurance copay-especially if you have a high deductible or your drug isn’t covered. You can choose to use either your insurance or the GoodRx discount, but not both. Always compare both prices before paying.
Do all pharmacies honor GoodRx coupons?
Most major chains like CVS, Walgreens, and Kroger honor GoodRx prices, but independent pharmacies may not. Some pharmacies don’t update their systems in real time, so the price you see on the app might not match what’s in their system. Always call ahead or ask the pharmacist to verify the price before you pay.
Are there free programs to get cheap or free generic drugs?
Yes. RxAssist.org is a free database that lists manufacturer patient assistance programs. Many drug companies offer free or low-cost generics to people who qualify based on income. In 2024, 78% of applicants who used RxAssist successfully got their medication. The application process can be complex, but many programs have staff to help you fill out forms.
Why doesn’t my insurance always show the lowest price?
Insurance plans use formularies that prioritize certain drugs based on rebates, not price. A drug might be covered at a low copay because the manufacturer pays a big rebate to your insurer-not because it’s the cheapest option. That’s why using a tool like GoodRx or asking your pharmacist for the cash price can reveal a lower cost than your insurance allows.
Should I ask my doctor to prescribe a cheaper alternative?
Absolutely. Doctors often prescribe what’s familiar or what’s listed first in their system. But if you ask, “Is there a generic version? Is there a cheaper one that works just as well?” they can usually switch you. Studies show that when doctors use real-time pricing tools, they prescribe cheaper alternatives 8.2% more often-without lowering effectiveness.


Just used GoodRx for my metformin this morning. $3.50 at the CVS down the street. My insurance copay was $22. I didn’t even need to call my doctor. Walked in, showed the app, paid cash, walked out. Why do people still let insurance dictate their pharmacy choices?
Let me guess-you think this is about transparency? Nah. This is about the entire pharmaceutical-industrial complex being a rigged casino where the house always wins, and you’re the sucker holding the losing ticket. The ‘cash price’ you see on GoodRx? That’s the price they want you to pay so you don’t ask why the net price is $1.20. The rebates? They’re not hidden because of bureaucracy-they’re hidden because if you knew how much Big Pharma was pocketing after the PBM skim, you’d torch the whole system. And no, asking your pharmacist won’t fix it. They’re just middlemen with a paycheck tied to the same broken machine.
Meanwhile, the FDA approves generics that are chemically identical but somehow cost 10x more in Nebraska than in Oregon. Why? Because no one’s auditing the supply chain. No one’s holding manufacturers accountable. And until we nationalize drug pricing or break up PBMs, all these ‘tools’ are just digital bandaids on a hemorrhaging artery.
Oh, and ‘RxAssist.org’? Cute. A nonprofit database that helps people get free medicine because the system failed them. That’s not empowerment-that’s charity in a system designed to make you need it.
Okay but have you ever tried using GoodRx at a small independent pharmacy? I did last week-showed the app, the guy just shrugged and said ‘we don’t honor those.’ No explanation, no apology. Just ‘sorry, man.’ Then I asked for the cash price and it was $18. Same drug. Same dose. Same day. I just stood there like an idiot. Feels like we’re all playing a game where the rules change every time you walk in the door.
I switched to a 90-day supply of my blood pressure med last month and saved $60. Simple move, huge difference. Also, always ask for the cash price-even if you have insurance. It’s not magic, just common sense.
GoodRx? Please. That’s just a front. The same companies that run GoodRx are owned by the same PBMs that control your insurance. They show you low prices so you think you’re winning, but they’re still getting paid behind the scenes. They want you to think you’re saving money so you don’t look at the bigger picture: your data, your prescriptions, your health-all being monetized by a cartel. And don’t get me started on how the government lets them get away with it.
The system is rigged!! The PBM’s are the real villains-these corporate vultures-stealing from you while pretending to help!! They manipulate rebates, inflate list prices, and then laugh while you pay $45 for a pill that costs 87 cents to make!! The FDA is in on it!! The CDC is in on it!! They don’t want you to know the truth!! YOU’VE BEEN PROGRAMMED TO BELIEVE IN ‘TRANSPARENCY’-BUT TRANSPARENCY IS A TRAP!! THEY WANT YOU TO THINK YOU’RE IN CONTROL-WHILE THEY STILL OWN THE GAME!! READ THE FEDERAL REGISTER!! LOOK AT THE STOCK TRANSACTIONS!! IT’S ALL THERE!! THEY’RE LAUGHING AT YOU RIGHT NOW!!
It’s not about price-it’s about control. The entire pharmaceutical system was designed to make you dependent. You think you’re saving money with GoodRx? You’re just participating in the illusion of choice. The real cost isn’t what you pay-it’s what you stop questioning. You don’t ask why your doctor prescribes the same drug every time. You don’t ask why the same pill costs different amounts in the same town. You don’t ask why the government won’t negotiate. You just accept it. And that’s the real tragedy.
People think transparency fixes everything. But transparency without accountability is just theater. And we’re all just watching the show.
I like how this post breaks it down without being preachy. Honestly, the biggest win for me was just asking my pharmacist for the cash price. I used to just hand over my card and assume it was the best deal. Turns out, I was overpaying by like 300%. Now I check GoodRx before I go, and sometimes I even call ahead. It takes 2 minutes. Saves me $50 a month. Doesn’t fix the system, but it lets me not get robbed every time I need my meds.
Also-90-day supplies? Game changer. If your pharmacy doesn’t offer it, ask. Most do.
Interesting how everyone’s excited about ‘tools’ but no one talks about the root: capitalism with no teeth. You can use GoodRx all you want, but the fact that a 30-day supply of insulin costs $4 in Canada and $300 here? That’s not a pricing glitch-that’s a moral failure. And the fact that we treat this like a personal responsibility issue-‘just ask your pharmacist!’-is the real scam. This isn’t about you being smart. It’s about a system that lets corporations profit from sickness. And until we stop pretending that individual action can fix structural corruption, we’re just rearranging deck chairs on the Titanic.
Also, the PBM rebate system? It’s a classic incentive misalignment. Why would a company lower the list price if higher prices = bigger rebates = bigger profits? They’re incentivized to make drugs more expensive. The whole thing is a Ponzi scheme disguised as healthcare.
So yes, use the tools. But don’t mistake them for justice.
This is the kind of info that actually helps. I used to panic every time I had to refill my meds. Now I know to check GoodRx, ask for cash price, and always ask my doctor if there’s a cheaper option. Small steps, but they add up. You don’t need to fix the whole system-you just need to know your options.
William Liu said it best. Small steps matter. I used to feel helpless. Now I feel like I have power-even if it’s just knowing to ask for the cash price. That’s not nothing.