Diabetes Combination Medications: Generic Options and Substitution Guide

Managing Type 2 diabetes often means taking more than one pill a day. For many people, that adds up to four, five, or even six pills-each with different schedules, side effects, and costs. That’s where diabetes combination medications come in. These pills bundle two or more drugs into a single tablet, cutting down on pill burden and making it easier to stick with treatment. But here’s the real question: when your doctor prescribes a brand-name combo, can you switch to a cheaper generic? And if you do, will it still work?
What Are Diabetes Combination Medications?
Diabetes combination medications aren’t new, but they’ve become essential tools in long-term care. They typically pair metformin-with its proven ability to lower liver glucose output and improve insulin sensitivity-with a second drug that works in a different way. Think of it like a two-pronged attack on high blood sugar. One drug handles insulin resistance, the other boosts insulin production, slows digestion, or helps the kidneys flush out extra glucose. The most common combos you’ll see are:- Metformin + DPP-4 inhibitor (like sitagliptin in Janumet)
- Metformin + SGLT2 inhibitor (like empagliflozin in Synjardy)
- Metformin + sulfonylurea (like glipizide in Metaglip or glyburide in Glucovance)
Why Generic Versions Matter
Brand-name combo pills can cost hundreds of dollars a month. Janumet, for example, ran close to $500 before generics entered the market. Synjardy? Still over $580 for a 30-day supply. That’s not just expensive-it’s a barrier to care. Generic versions change the game. Take Metaglip (glipizide/metformin). The brand version is gone. But the generic? Around $18 for 60 tablets. That’s a 95% drop in price. Glucovance (glyburide/metformin) is even cheaper at $15. These aren’t just affordable-they’re life-changing for people on fixed incomes. But here’s the catch: not all combos have generics. Only five out of 25 available combination medications in the U.S. have generic equivalents as of late 2023. The newer ones-especially those with SGLT2 or DPP-4 inhibitors-are still locked behind patents. Synjardy won’t have a generic until at least 2026. Janumet XR is still brand-only too, even though its main patent expired in early 2024. Formulation patents can delay generics for years.When Generic Substitution Works Well
Not all combo meds are created equal when it comes to switching. The older, simpler combinations tend to transition smoothly. That’s because their components have been around for decades. Metformin has been generic since the 1980s. Glipizide and glyburide? Generic for over 20 years. A 2022 Joslin Diabetes Center survey found that 76% of patients who switched from brand to generic Metaglip or Glucovance saw no change in blood sugar control. Many reported the same side effects-or even fewer. On Reddit’s r/Diabetes, 42% of 247 respondents said their blood sugar stayed stable after switching. That’s a strong signal: for stable, long-term users, generics are reliable. Pharmacists see it too. Generic versions of these older combos meet the FDA’s bioequivalence standards: they deliver the same amount of drug into the bloodstream within an acceptable range (80-125% of the brand). For metformin and sulfonylureas, that’s enough. The body responds predictably.
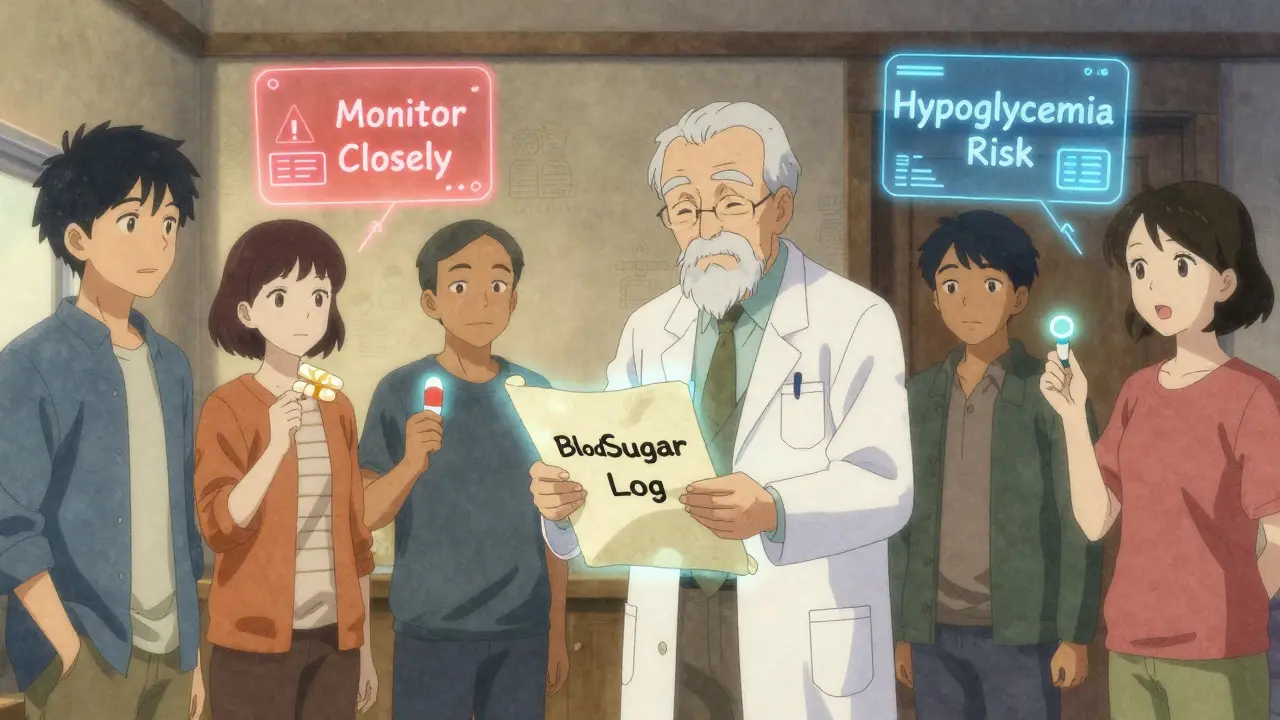
When Substitution Gets Risky
But not all combos are this forgiving. The problem comes with drugs that have a narrow therapeutic window-where even a small change in blood levels can cause problems. Glyburide, for example, is one of those. A user on Diabetes Daily shared how switching from brand Glucovance to generic triggered repeated low blood sugar episodes. Why? The generic version released glyburide slightly faster. That tiny difference was enough to push blood sugar too low. That’s not an isolated case. A 2022 American Pharmacists Association survey found that 12% of pharmacists had heard reports of patients experiencing unexpected side effects after switching diabetes combos. Endocrinologists are cautious. Dr. John Buse from UNC wrote in Diabetes Care that the 80-125% bioequivalence range might be too wide for some diabetes drugs. A 15% dip in drug levels might not matter for a painkiller-but it could mean the difference between good control and dangerous highs. Also, generics usually come only in immediate-release (IR) form. If your doctor prescribed Janumet XR (extended-release), the generic version likely won’t have that option. Extended-release formulations are designed to release the drug slowly over time-reducing stomach upset and evening spikes. Switching to IR might mean more nausea, more frequent dosing, or worse glucose swings.What to Do Before You Switch
Don’t just swap pills at the pharmacy. Even if your insurance pushes you to the cheapest option, you need a plan. Start with your doctor. Ask:- Is this combo made of older, well-studied drugs?
- Am I on an extended-release version? Is there a generic XR?
- Have I had any recent blood sugar swings or side effects?
- Get a new prescription clearly marked with the generic name (e.g., “glipizide/metformin” not “Metaglip”).
- Check the pill appearance. Generics often look different-color, shape, imprint. Take a photo so you know what to expect.
- Test your blood sugar more often for the first 2-4 weeks. Aim for 4 checks a day: fasting, before meals, and at bedtime.
- Keep a log. Note any changes in energy, hunger, dizziness, or stomach issues.
- Call your doctor if your fasting sugar jumps above 140 mg/dL for three days in a row, or if you have two episodes of low blood sugar (below 70 mg/dL).
Insurance, Costs, and Hidden Barriers
Even if a generic exists, your insurance might not cover it right away. Sixty-three percent of patients in a 2023 ADA survey said they had to fight for coverage-through prior authorization, step therapy, or appeals. Here’s the trick: many brand-name manufacturers offer copay cards that cut monthly costs to $0 for eligible patients. Teva, Mylan, and Sandoz-the big generic makers-rarely do. Their business model is low price, low support. You’re on your own. If you’re struggling with cost, ask your pharmacist about patient assistance programs. Some nonprofits, like NeedyMeds or RxAssist, can help you get free or discounted meds-even if you’re not on Medicaid.The Future: More Generics Coming
The tide is turning. Jentadueto (linagliptin/metformin) got its first generic approval in May 2023, though it won’t hit shelves until 2025. Janumet XR’s patent expires fully in 2026. That means within the next two years, several more combo meds will drop in price. By 2030, experts predict the generic segment will grow at nearly twice the rate of branded combos. The Congressional Budget Office estimates that as these older combos go generic, the average annual cost for a diabetes combination could fall from $2,850 to just $420. That’s not just savings. It’s access. It’s fewer people skipping doses because they can’t afford it. It’s fewer hospital visits from uncontrolled sugar.Bottom Line: Can You Switch?
Yes-but not always. For older combos like Metaglip and Glucovance, switching to generic is safe, effective, and smart. For newer ones like Synjardy or Janumet XR, wait until generics arrive. Don’t let a pharmacy substitute without checking with your doctor first. If you’re stable, on a simple combo, and cost is a problem-go generic. Monitor closely. Keep records. Talk to your care team. If you’re new to meds, have unstable blood sugar, or need extended-release-stick with the brand until you’ve had time to understand how your body responds. Your health isn’t a cost center. It’s your foundation.Can I switch from a brand-name diabetes combo to a generic without my doctor’s approval?
No. Even if your pharmacy automatically substitutes a generic, you should always inform your doctor. Some diabetes medications, especially sulfonylureas, have narrow therapeutic windows where small changes in blood levels can cause hypoglycemia or reduced effectiveness. Automatic substitution without clinical oversight has led to treatment failures in nearly 19% of cases, according to the American Association of Clinical Endocrinology.
Are generic diabetes combo pills as effective as brand names?
For older combinations like metformin/glipizide or metformin/glyburide, yes-most patients see the same blood sugar control. These drugs have been used for decades, and their generics meet FDA bioequivalence standards. But for newer combos like those with SGLT2 or DPP-4 inhibitors, generics aren’t available yet. Even among available generics, some patients report minor differences in side effects or absorption, which is why close monitoring after switching is essential.
Why are some diabetes combo meds still brand-only?
Patents protect new drug combinations for up to 20 years from the date of filing. Many newer combos, like Synjardy (empagliflozin/metformin) or Janumet (sitagliptin/metformin), are still under patent. Even after the main patent expires, companies often file additional patents on formulations (like extended-release versions), which can delay generics for several more years. As of 2026, only five out of 25 combination diabetes medications have generic versions available in the U.S.
Do generic diabetes combos have the same side effects as brand names?
The active ingredients are identical, so the same side effects are possible-like nausea, diarrhea, or low blood sugar. But some patients report differences due to inactive ingredients (fillers, coatings) or release timing. For example, switching from an extended-release brand to an immediate-release generic can cause more stomach upset. In rare cases, faster absorption of sulfonylureas in generics has led to unexpected hypoglycemia. Always monitor blood sugar closely after switching.
How long should I monitor my blood sugar after switching to a generic?
The American Association of Clinical Endocrinology recommends checking your blood sugar four times daily for 2 to 4 weeks after switching. Test fasting, before meals, and at bedtime. If your numbers become erratic-two low readings under 70 mg/dL or three days over 140 mg/dL fasting-contact your doctor. Don’t wait. Adjustments may be needed in diet, timing, or dosage.
Can I get help paying for brand-name diabetes combos if I can’t afford the generic?
Yes. Many brand-name manufacturers offer copay cards that reduce monthly costs to $0 for eligible patients-even if you have insurance. Programs from companies like Merck, Boehringer Ingelheim, and Janssen can cover up to 100% of the cost. Visit their websites or ask your pharmacist for details. If you’re low-income, nonprofit programs like NeedyMeds or RxAssist can connect you with free or discounted medications.


Bro i switched my Janumet to generic and my sugar went nuts for two weeks. Pharmacist didn't even tell me it was IR not XR. Now i'm back on brand and my HbA1c is down. Don't let them pull that crap on you.
Let me tell you something about generics - they're not just cheaper, they're revolutionary. I was paying $450/month for Synjardy until the generic came out. Now I pay $18. I've been stable for 14 months. The system wants you to stay sick so they can keep selling you $500 pills. Don't let them win. Track your numbers, yes - but don't be afraid to fight for your health.
From a clinical pharmacology standpoint, the bioequivalence window of 80-125% is indeed problematic for drugs with narrow therapeutic indices like sulfonylureas - particularly glyburide, which has nonlinear pharmacokinetics and high interpatient variability. The FDA's standard was designed for analgesics and antihypertensives, not for agents where a 15% fluctuation in Cmax can precipitate hypoglycemic events. The 2022 APhA data showing 12% of pharmacists reporting adverse events post-substitution isn't noise - it's a systemic failure in regulatory harmonization. We need pharmacovigilance protocols specific to diabetes combos, not just blanket substitution policies driven by PBM cost-cutting.
America is being sold a lie. The pharmaceutical industry doesn't care about your health - they care about your wallet. They patent the *formulation*, not the *medicine*. They make you believe that the difference between a blue pill and a yellow pill is science - when it's just lawyers and lobbyists. The real innovation isn't in the drug - it's in the patent extensions. We're not fighting diabetes. We're fighting capitalism disguised as medicine.
So you're telling me I should risk my life because the pharmacy wants to save $480 a month? Cool. I'll just keep paying for the brand. My A1c is 5.8. Your generic might be 6.2. Who's the hero now? 😎
Hey, I switched to generic Glucovance last year and honestly? It was fine. I monitored my sugars like crazy for a month - morning, before lunch, before dinner, bedtime. No crashes, no spikes. My doc said I'm doing better than most people on brand. I know it sounds scary, but if you're stable and your combo is old-school (metformin + sulfonylurea), it really works. Just don't skip the check-ins. You got this 💪
I'm from the U.S., but I've lived in Canada and India - and I've seen how this plays out differently. In Canada, generics are automatic and monitored. In India, they're dirt cheap and widely trusted. Here? We're stuck in this weird limbo where the system says "trust the science," but the pharmacy says "take the cheapest," and your doctor isn't always in the loop. We need better communication - not just between doc and patient, but between pharmacy systems and EHRs. This isn't about money. It's about coordination.
My mom switched to generic and her sugar went wild. She didn't tell anyone for weeks. Now she's in the hospital. Just saying.
It's not about generics being bad - it's about the system being broken. People are being forced into choices they don't understand. Doctors don't have time to explain. Pharmacists are incentivized to swap. Insurance companies don't care if you end up in the ER. This isn't healthcare - it's a numbers game. And the people paying the price? They're the ones who can't afford to lose.
Let’s be real - if you’re on a combo with SGLT2 or DPP-4, you’re already paying for luxury. The brand names? They’re the Tesla of diabetes meds. Generics are the Honda. Both get you there. But if you’re racing? Stick with the Tesla. If you’re just commuting? The Honda’s fine. Just don’t pretend the Tesla is a scam. It’s not. It’s just expensive. And that’s okay - if you can afford it.
Think about it: we’ve been told for decades that generics are just as good. But when your life depends on a drug that has to be absorbed just right - not 15% more, not 15% less - then "just as good" becomes a dangerous lie. The FDA’s standards were written for aspirin, not for drugs that keep you alive. We need to stop pretending that all medicines are created equal. Some are. Most aren’t. And we owe it to patients to admit that.
Oh wow, so the solution to America’s healthcare crisis is… to let people die because they can’t afford insulin? Or is it to let them crash from hypoglycemia because the generic made glyburide hit faster? Maybe we should just stop pretending this is about health and admit it’s about profit. The real question isn’t "can you switch?" - it’s "why does this even exist?"
Generics work for some. They don’t for others. The data is messy. The system is broken. You’re on your own.