Diabetes and Exercise: How to Prevent Low Blood Sugar During Workouts

Working out with diabetes doesn’t have to mean avoiding exercise because you’re scared of crashing. But if you’ve ever felt shaky, sweaty, or dizzy mid-run - and your meter reads 65 mg/dL - you know the fear is real. About half of people with type 1 diabetes skip workouts just because they’re afraid of low blood sugar. The good news? You can train safely. It’s not about avoiding activity. It’s about planning it right.
Why Exercise Drops Your Blood Sugar
When you move, your muscles don’t wait for insulin to grab glucose. They pull it straight from your bloodstream to fuel movement. That’s a good thing - it helps lower blood sugar naturally. But for someone on insulin, this extra demand can tip the scales too far. Your body also becomes more sensitive to insulin for up to three days after a workout. So even if your glucose looks fine before you start, it might drop hours later - even while you’re sleeping.Check Before You Start
Don’t just guess. Check your blood sugar 15 to 30 minutes before you begin. Here’s what to do based on the number:- Below 90 mg/dL: Eat 0.5 to 1 gram of carbs per kilogram of body weight. For a 70 kg person, that’s 35 to 70 grams of carbs - think two bananas or a large granola bar.
- 90-150 mg/dL: Still eat 0.5-1 g/kg carbs before starting. Don’t skip this just because you think you’re "fine."
- Below 100 mg/dL: The American Diabetes Association recommends at least 15-20 grams of fast-acting carbs. Wait 15 minutes, check again. If it’s still low, eat another 15 grams.
Timing Matters More Than You Think
When you take insulin isn’t just about meals. It’s about movement. If you take a bolus at 8 a.m. and hit the gym at 10 a.m., you’re working out right when that insulin is peaking. That’s a recipe for a crash. Instead, aim to exercise when your insulin is stable - usually 2-4 hours after a meal. If you’re on a pump, look at your insulin-on-board (IOB). If you have more than 1.2 active units, your risk of low blood sugar jumps. That’s because during exercise, each unit acts like 2-3 units. One small bolus can turn into a big problem.Not All Workouts Are Created Equal
A 30-minute jog? That’s a slow, steady glucose drop. But if you add a 10-second all-out sprint before or after? It can stop the drop cold. That’s because high-intensity bursts trigger adrenaline, which tells your liver to dump glucose into your blood. Same goes for lifting weights. A 45-minute strength session before cardio cuts glucose decline by almost half. One study showed people who did resistance first dropped from 166 to 124 mg/dL - compared to 166 to 105 mg/dL without it. That’s a 20-point buffer.HIIT and Circuits - Use Them Wisely
High-intensity interval training (HIIT) - think 30 seconds sprint, 90 seconds walk - actually reduces hypoglycemia risk during and after. A 2019 study found glucose stayed stable for up to 45 minutes post-workout. But circuit training? That’s trickier. If you’re moving fast with little rest, your muscles keep burning glucose without the adrenaline spike to balance it. That can still cause lows. So if you’re doing circuits, check more often. And never skip the post-workout snack.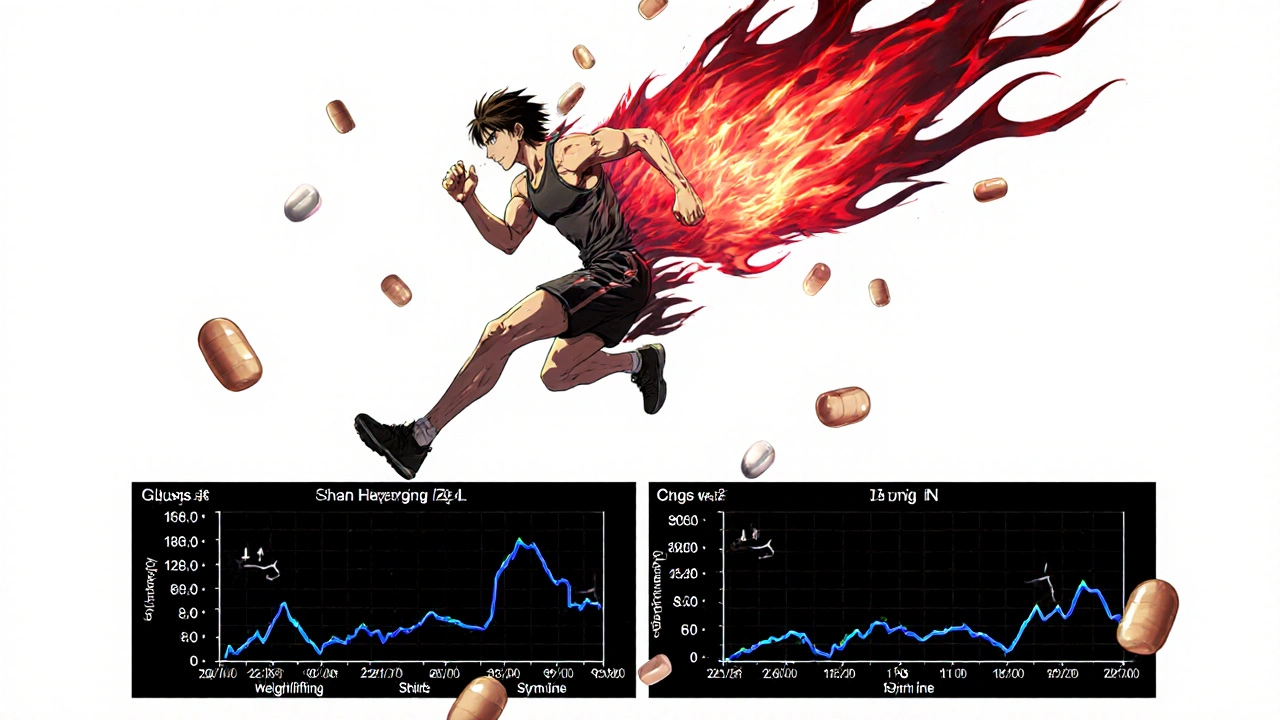
What to Eat and When
Carbs aren’t just for before. You need them during long sessions. For workouts longer than 60 minutes, eat 15-30 grams of carbs every hour. Think: half a banana, a handful of gummies, or a sports drink. And don’t wait until you feel low. Proactive fueling beats reactive fixing. For overnight protection, especially after afternoon or evening workouts, eat a bedtime snack with 15 grams of carbs plus a little protein. A small apple with peanut butter or a cup of Greek yogurt with berries works. Why? Delayed hypoglycemia hits 70% of people with type 1 diabetes. You might feel fine at 10 p.m., but crash at 2 a.m. That’s not luck - it’s biology.Technology Can Help - But It’s Not Magic
If you use a CGM, you’re already ahead. Dexcom’s G7 has an "exercise mode" that lowers alert thresholds by 20 mg/dL during activity. That means you get warned earlier. But even the best tech can’t predict everything. One user on Reddit said he did the exact same 5K run, at the same time, with the same insulin on board - and got 70 one day and 180 the next. That’s normal. Your body changes. Sleep, stress, weather, hormones - they all shift how you respond. New pumps like the Tandem t:slim X2 now have an "Exercise Impact" feature. It uses machine learning to predict glucose drops based on your history and the workout you’re about to do. It can automatically reduce insulin delivery. That’s huge. But it’s still new. Most people still rely on manual adjustments.Adjusting Insulin for Workouts
If you’re on an insulin pump, reduce your basal rate by 50-75% starting 60-90 minutes before moderate exercise. For example, if your normal basal is 1.0 unit/hour, drop it to 0.25-0.5 for the next few hours. If you’re on multiple daily injections, reduce your pre-workout bolus by 25-50%. Don’t just guess - track it. Write down what worked last time. Your body remembers patterns better than you think.What People Are Actually Doing
On T1D Exchange, 78% of users use temporary basal reductions before exercise. Of those, 63% say it works. On Reddit, people swear by pre-workout sprints. One user went from four lows a week to one every two weeks just by adding a 10-second bike sprint before his run. Another said he stopped night lows after starting a bedtime snack with protein. These aren’t outliers. They’re people who learned by doing.
The Learning Curve Is Real
Don’t expect to master this in a week. It takes 3-6 months of consistent tracking to understand your body’s response to different workouts. Start small. Try one new activity at a time. Check your glucose every 15 minutes during the first few sessions. Log everything: what you ate, how much insulin you took, how hard you worked, and your glucose before, during, and after. Over time, you’ll see the patterns.When to Stop and What to Carry
Always carry fast-acting carbs. Glucose tabs, juice boxes, gummies - something you can grab fast. Don’t rely on your phone or gym bag. Keep it in your pocket. If your glucose drops below 70 mg/dL during exercise, stop. Eat 15 grams. Wait 15 minutes. Check again. Don’t push through. A low can turn into a severe one fast.What to Do After
Your work isn’t done when you finish. Check your glucose again 1-2 hours after. And if you exercised in the afternoon or evening, check before bed and possibly once during the night. Set an alarm if you need to. Delayed lows are the silent killer.It’s Not About Being Perfect
Some days you’ll nail it. Other days, you’ll crash anyway. That’s okay. The goal isn’t perfection. It’s consistency. You don’t need to avoid exercise. You need to plan for it. Every low you prevent is a win. Every workout you complete without a crash is progress.Final Thought
Exercise isn’t the enemy. Fear is. You can run, swim, lift, bike - and stay safe. It just takes a little prep, a little patience, and a lot of data. Start with one change: check your glucose before your next workout. Then add one more thing next time. Slowly, you’ll build confidence. And your body will thank you.Can I exercise if I have type 2 diabetes and take insulin?
Yes. People with type 2 diabetes who use insulin face the same hypoglycemia risks as those with type 1. The same rules apply: check your blood sugar before, during, and after exercise. Adjust insulin if needed. Carry fast-acting carbs. The key is understanding how your body responds - not your diabetes type.
Do I need to eat carbs before every workout?
Not always. If your blood sugar is above 150 mg/dL and you’re doing light activity like a short walk, you may not need extra carbs. But for anything moderate to intense - cycling, running, lifting - and if your glucose is below 150 mg/dL, eat something. Better safe than low.
Why do I get low after exercise, even when I ate?
Because exercise keeps your muscles hungry for glucose for hours - sometimes up to 72 hours. Even if you ate before, your body is still using more insulin and pulling glucose from your blood. That’s why delayed lows happen. Check your glucose before bed and consider a small snack with carbs and protein.
Should I reduce my insulin before a workout?
For most people using insulin, yes. If you’re on a pump, reduce your basal rate by 50-75% starting 60-90 minutes before exercise. If you use injections, reduce your pre-workout bolus by 25-50%. This prevents insulin stacking during activity. Always track what works for you.
Can continuous glucose monitors (CGMs) prevent lows?
They don’t prevent lows - but they give you early warnings. CGMs like Dexcom G7 adjust alerts during exercise, so you see drops before they become dangerous. They’re not foolproof, but they’re the best tool you have. Pair them with smart carb intake and insulin adjustments for the best results.
Is it safe to exercise on an empty stomach?
It’s risky if you’re on insulin. Even if your glucose is normal, insulin on board can still cause a drop. For safety, always check your blood sugar and have carbs nearby. If you’re doing light activity like walking and your glucose is above 150 mg/dL, you might be okay - but never assume.
What’s the best type of exercise for preventing lows?
Combining resistance training with aerobic exercise works best. Lifting weights before running or cycling reduces glucose drops significantly. Short sprints (10-15 seconds) before or after aerobic activity also help. Avoid long, steady-state cardio alone if you’re prone to lows.
How long should I wait after eating to exercise?
Wait 2-4 hours after a meal to avoid peaking insulin during exercise. If you eat a snack before working out, wait 30-60 minutes. Use your insulin-on-board reading to guide you - if you still have active insulin, delay your workout.
Can I drink alcohol before or after exercise?
Avoid alcohol before or after exercise. Alcohol blocks your liver from releasing glucose, which increases hypoglycemia risk - especially overnight. If you drink, check your glucose more often and eat extra carbs. Never exercise after drinking without a plan.
What should I do if I have a severe low during exercise?
Stop immediately. If you’re conscious, consume 15-20 grams of fast-acting carbs. Wait 15 minutes. If you’re confused, unable to swallow, or unconscious, someone must give you glucagon. Always carry a glucagon kit and make sure your workout partner knows how to use it. Never ignore a severe low.



Pre-workout carbs? Nah. Just spike your glucagon like a proper adult. You’re not a toddler with a juice box. Your liver’s got a job to do - stop treating it like a vending machine.
Also, if you’re checking glucose every 15 minutes, you’re not training - you’re data-mining your own panic.
Real athletes just eat, move, and trust their bodies. Or don’t. I’m not your coach.
Also, why are you even on insulin if you’re this scared of a number?
Just saying.
It is imperative to emphasize that the physiological mechanisms underlying exercise-induced hypoglycemia are well-documented in peer-reviewed literature, particularly in the context of insulin pharmacokinetics and muscle glucose uptake dynamics.
Pre-exercise carbohydrate ingestion, when blood glucose is below 150 mg/dL, is strongly supported by the American Diabetes Association’s 2023 Standards of Care.
Furthermore, the reduction of basal insulin rates by 50–75% for moderate-intensity aerobic activity is a clinically validated strategy, as demonstrated in randomized controlled trials by the Diabetes Technology Society.
It is also essential to note that delayed hypoglycemia may occur up to 72 hours post-exercise due to enhanced insulin sensitivity, necessitating nocturnal monitoring.
Compliance with these evidence-based protocols significantly reduces the incidence of severe hypoglycemic events.
Patients are encouraged to maintain detailed glycemic logs and consult with certified diabetes care and education specialists for individualized regimens.
They told you to eat carbs before exercise. But what they didn’t tell you is that insulin is a poison disguised as medicine.
Big Pharma wants you dependent. They want you checking your CGM every 10 minutes.
Real solution? Stop injecting synthetic hormones. Go keto. Go fasting. Your liver doesn’t need your help.
Also, HIIT? That’s just a scam to sell you protein powder and glucose tabs.
Exercise is supposed to make you strong - not addicted to gummies.
Wake up.
While the post provides a comprehensive overview of exercise-induced hypoglycemia mitigation strategies, I would like to inquire about the applicability of these recommendations across diverse insulin regimens - particularly in patients utilizing long-acting analogs such as degludec or glargine U300.
Is the 50–75% basal reduction still appropriate in the context of ultra-long-acting insulins with minimal peak activity?
Additionally, are there any studies evaluating the efficacy of pre-exercise protein supplementation in attenuating post-exercise glucose declines, particularly in the context of resistance training?
Further clarification on these points would be greatly appreciated.
They’re hiding something.
Why does Dexcom’s ‘exercise mode’ lower thresholds by exactly 20 mg/dL? Coincidence? I think not.
That’s the same number they use in the FDA’s ‘glucose stability’ testing protocol - the one that got the old sensors recalled in 2018.
And the Tandem pump’s ‘Exercise Impact’ feature? That’s not machine learning - it’s a backdoor.
They’re tracking your workouts. Your insulin use. Your sleep. Your carbs.
They’re building a profile.
Next thing you know, your insurance will raise your rates because you ‘had too many lows.’
Don’t be fooled. This isn’t health tech - it’s surveillance disguised as help.
YESSSSS this is everything!!! 🙌🔥
Just did a 45-min lift + 20-min run and I’m still at 130 😍
Pre-workout sprint was the MVP 🏃♀️💥
Also ate an apple with peanut butter before bed and slept like a baby 🌙🍎🥜
You guys are LEGENDS for sharing this!!
Finally feel like I’m not fighting my own body 💪❤️
Wow. So much advice. So many numbers. So much fear wrapped in a ‘guide.’
Let me get this straight - you’re telling me I need to calculate carbs per kilogram, track insulin-on-board, adjust basals, monitor for 72 hours, carry gummies in my pocket, set alarms, and still, I might crash anyway?
And this is supposed to make me feel empowered?
What if I just… don’t want to do all this math just to go for a walk?
It’s okay to be tired of managing this. It’s okay to want to just move without a spreadsheet.
You’re not broken. You’re just exhausted.
And that’s valid.
Maybe the real solution isn’t more rules.
Maybe it’s permission to rest.
And maybe, just maybe, it’s okay to skip the workout today.
You’re not failing. You’re human.
I’ve been doing the pre-workout sprint thing for 3 months now and it’s been a game changer 🤯
Used to crash 3x a week now barely even dip below 90
Also the bedtime apple + peanut butter saved my nights 😴🍎
Don’t forget to check 2 hours after even if you feel fine
My CGM showed a drop at 2am that I would’ve missed if I didn’t set the alarm
Also I use the Dexcom G7 and it’s so much better than my old one
Trust the data but don’t let it own you
Progress not perfection baby 💪❤️
Oh, so now we’re all supposed to be glucose accountants? How charming.
You’ve turned a simple act of movement into a high-stakes financial audit.
‘Eat 0.5 to 1 gram per kilogram’ - so if I’m 60kg, that’s 30g carbs. If I’m 80kg, that’s 80g. You’re not prescribing nutrition - you’re prescribing guilt.
And the ‘delayed lows’? That’s just the system’s way of keeping you dependent.
But hey - at least your CGM has a ‘smart’ alert. Maybe next it’ll text your boss to say you’re ‘too unstable to work today.’
How poetic. You’re not sick. You’re a data point.
Wow. Linda just said what everyone’s thinking but won’t admit.
And now I feel seen.
Also, I just walked 2 miles yesterday. Didn’t check. Didn’t eat. Didn’t care.
Glucose was 110.
Still alive.
Maybe the real hack is… not overthinking it.
Just move. Then eat. Then sleep.
Repeat.