Uremic Symptoms: Nausea, Itch, and When to Start Dialysis

When your kidneys stop working, your body doesn’t just slow down-it starts poisoning itself. The waste products that should be flushed out begin to pile up, and that’s when uremic symptoms show up. Nausea, relentless itching, metallic taste in your mouth, fatigue so deep it feels like you’re dragging concrete-these aren’t just inconveniences. They’re your body screaming for help. And if you’re living with advanced kidney disease, ignoring them can cost you more than comfort-it can cost you time, health, and even life.
What Exactly Is Uremia?
Uremia isn’t a disease. It’s the result of one. When your kidneys drop below 10-15% of normal function, they can no longer filter out toxins like urea, creatinine, and indoxyl sulfate. These aren’t just numbers on a lab report-they’re chemicals that build up in your blood and start messing with your brain, skin, gut, and heart. The term comes from "urea," a waste product from protein breakdown, but the real problem is the whole cocktail of toxins your kidneys used to remove. Back in the 1800s, uremia meant death. People waited until they were barely conscious before doctors would act. Then, in 1943, Willem Kolff built the first working dialysis machine in the Netherlands using sausage casings and juice cans. It saved lives. Today, we have better machines, better drugs, and better understanding-but too many people still wait too long.Nausea: More Than Just an Upset Stomach
If you’ve ever felt like your stomach is full of rocks and every bite of food feels wrong, you might be dealing with uremic nausea. It’s not just indigestion. It’s your brain being tricked. Toxins like p-cresyl sulfate and indoxyl sulfate cross the blood-brain barrier and hit the chemoreceptor trigger zone-the part of your brain that controls vomiting. Studies show 68% of people with stage 5 chronic kidney disease (CKD) report nausea, and 92% of them say it started between 6 and 12 weeks before they started dialysis. This isn’t mild discomfort. People describe it as constant, unrelenting. One patient on a kidney forum wrote: "I lost 18 pounds in two months because eating felt like swallowing sand." Food loses its taste. Protein-heavy meals become unbearable. Weight loss isn’t intentional-it’s survival. And when you’re already weak from kidney failure, losing muscle mass makes everything worse. Doctors treat this with ondansetron (Zofran), usually 4mg three times a day. For stubborn cases, domperidone might be used, but it carries heart risks. The real fix? Dialysis. Once toxins are cleared, nausea often lifts within days. But if you wait too long, the nausea becomes so severe that you can’t eat enough to stay alive-and that’s when dialysis becomes urgent, not optional.Itch That Won’t Quit: Uremic Pruritus
If you’ve ever scratched until your skin bled just to get a few seconds of relief, you know what uremic pruritus feels like. It’s not eczema. It’s not dry skin. It’s a deep, burning, crawling sensation that comes and goes, often worse at night. Around 70% of people on dialysis suffer from it. Even more surprising-37% of people not yet on dialysis already have it. Why does it happen? No one knows for sure, but inflammation plays a big role. People with severe itching have CRP levels nearly triple those without it. There’s also evidence that opioid receptors in the skin go haywire. The itch isn’t in your skin-it’s in your nerves and your brain. Doctors use the 5-D Itch Scale to measure it: Duration, Degree, Direction, Disability, Distribution. A score over 12 means severe. Over 15? That’s a red flag. One patient on Reddit said: "I scratched until I bled. My Fitbit showed my sleep score dropped from 85 to 42. I hadn’t slept through the night in three years." Treatment starts with optimizing dialysis. If you’re not getting enough waste removed per session (Kt/V below 1.4), itching won’t improve. Then come medications: gabapentin (starting at 100mg at night) is often the first try. If that fails, newer drugs like difelikefalin (Korsuva) or nalfurafine can cut itch scores by 30% or more in weeks. Difelikefalin works fast-some feel relief within 48 hours. But these drugs aren’t magic. They’re tools. And they only work if you’re getting the right dialysis.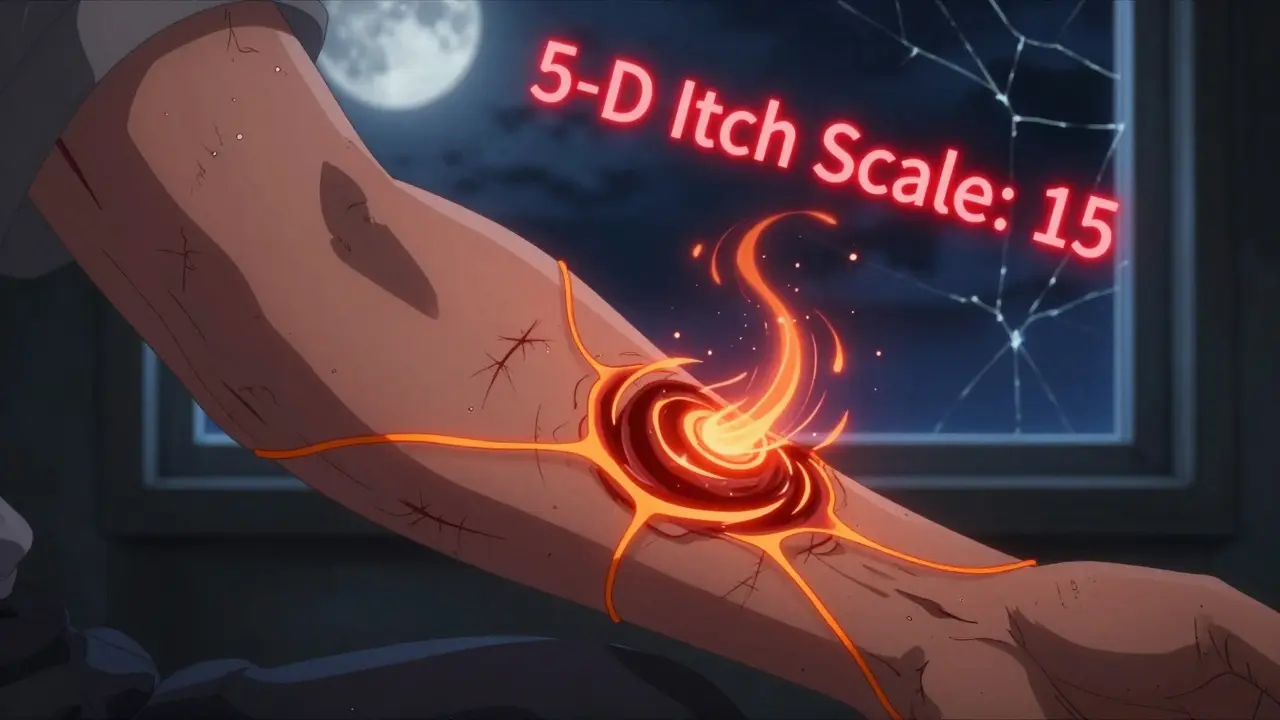
When Should You Start Dialysis?
This is the question that keeps nephrologists up at night. And for good reason. For decades, doctors waited until eGFR dropped below 5 or 6 mL/min before starting dialysis. Then came the IDEAL trial in 2010, which shook things up. It showed that starting dialysis earlier (eGFR 10-14) didn’t improve survival. In fact, patients who waited until symptoms appeared did just as well-if not better-when their symptoms were managed well. So what’s the new rule? Start dialysis when symptoms become unmanageable, not when a number hits a line. The 2023 KDOQI guidelines say dialysis should begin when:- eGFR is below 10.5 mL/min/1.73m² and
- BUN is above 70 mg/dL and
- Crucially-symptoms like nausea, itching, or fluid overload can’t be controlled with diet, meds, or better dialysis
What Happens If You Wait Too Long?
Waiting isn’t brave. It’s risky. The longer you delay dialysis with severe symptoms, the more damage you do. Nausea leads to malnutrition. Itching leads to infections from broken skin. Fluid overload leads to heart failure. And all of it increases your chance of ending up in the hospital. A 2022 study found that people with severe uremic pruritus had $8,432 higher annual medical costs-mostly because they ended up in the ER more often. One patient told a nurse: "I didn’t want to be a burden. I thought I could tough it out. By the time I called my doctor, I couldn’t stand up. They had to wheel me in on a gurney." And here’s the worst part: many people don’t get diagnosed until it’s too late. A 2022 University of Michigan poll found that 41% of patients with uremic symptoms saw three or more doctors before someone finally said, "Your kidneys are failing." The average delay? Over eight months.
What Can You Do Right Now?
If you have advanced kidney disease and are experiencing nausea or itching:- Track your symptoms. Write down when nausea hits, how bad the itch is, what makes it worse, and how it affects sleep or eating.
- Ask for the 5-D Itch Scale. Most nephrologists don’t use it unless you ask. Print it out. Fill it out. Bring it to your next appointment.
- Check your dialysis adequacy. If you’re already on dialysis, ask: "Is my Kt/V above 1.4?" If not, your sessions might be too short or too infrequent.
- Don’t accept "it’s just part of aging." Uremic symptoms are treatable. They’re not normal. You deserve to feel better.
- Speak up about weight loss. If you’ve lost more than 5% of your body weight in 3 months, that’s a medical emergency. Tell your doctor immediately.
What’s Changing in 2026?
The future of dialysis initiation is shifting-from numbers to how you feel. The 2024 KDIGO guidelines are expected to include patient-reported outcomes as official triggers. That means if your itch score is high, or your nausea keeps you from eating, your eGFR might not matter as much. New drugs like nemifitide are in late-stage trials, promising even better itch control without opioids. And research is finally focusing on why Black patients wait longer for dialysis-3.2 months on average-leading to higher hospitalization rates. This isn’t just about medicine. It’s about dignity. About sleep. About being able to eat a meal without gagging. About scratching without bleeding. Dialysis isn’t a failure-it’s a reset. And starting it at the right time means you get to live, not just survive.Can uremic itching go away without dialysis?
In early stages of kidney disease, yes-sometimes. Optimizing diet, controlling phosphate levels, using topical moisturizers, and taking gabapentin can help. But once you reach stage 5 CKD and symptoms are severe, dialysis is the only reliable way to remove the toxins causing the itch. Medications may reduce it, but they won’t eliminate it unless the root cause-the failing kidneys-is addressed.
Is nausea always a sign I need dialysis?
Not always. Nausea can come from many things-medications, stomach bugs, or even anxiety. But if you have advanced kidney disease and nausea is persistent, worsening, and affecting your appetite or weight, it’s a major red flag. When combined with high BUN levels (above 70 mg/dL), it strongly suggests uremia. Don’t wait for vomiting to start-talk to your nephrologist early.
Why do some doctors want to start dialysis earlier?
Some doctors believe preventing severe symptoms is better than treating them. A 2020 Japanese study showed fewer hospitalizations when dialysis started at eGFR 12-15. But large trials like IDEAL found no survival benefit. The debate isn’t about whether early dialysis helps-it’s about whether it’s worth the cost, time, and risk for patients who still feel okay. The goal now is to start when symptoms interfere with life, not just when a number drops.
What medications are safest for uremic nausea and itch?
For nausea: ondansetron is first-line. Domperidone works but carries heart risks. For itch: gabapentin is common and generally safe if dosed for kidney patients. Difelikefalin (Korsuva) is newer, effective, and FDA-approved for uremic pruritus-but requires monitoring for QT prolongation. Avoid opioids unless absolutely necessary. Always check dosing with your pharmacist-many drugs need adjustment for kidney failure.
How do I know if my dialysis is working well enough?
Ask for your Kt/V number after each session. For hemodialysis, it should be at least 1.4. If it’s lower, your sessions may be too short or too infrequent. Also track your weight between sessions-if you gain more than 4% of your dry weight, you’re likely retaining too much fluid. Talk to your dialysis team: they can adjust time, blood flow, or frequency. Better dialysis = fewer symptoms.
Can I delay dialysis if I feel okay?
If you have no symptoms and your eGFR is 8-10, yes-under close monitoring. But if you have even mild nausea, itching, poor sleep, or weight loss, you’re not "okay." Uremic symptoms are sneaky. They creep in slowly. By the time you feel bad, you’ve already lost muscle, sleep, and quality of life. Don’t wait for collapse. Talk to your doctor before symptoms get severe.


This post made me cry. I’ve been itching so bad I sleep with gloves on. My mom said I looked like a ghost. Then I started dialysis-and boom, I slept through the night for the first time in 2 years. 😭
It’s fascinating how modern medicine still treats uremia like a numbers game when it’s clearly a human experience. The body doesn’t care about eGFR-it cares about whether you can taste your coffee or scratch without bleeding. Maybe we need to stop measuring kidneys and start measuring dignity.
I think this is really important info. I had no idea that itching could be that severe before dialysis. I’ll make sure to print out the 5-D scale for my next appointment. Thanks for sharing.
From a nephrology standpoint, this is spot-on. The shift from eGFR-centric to symptom-driven initiation aligns with KDOQI 2023. Key metrics: Kt/V >1.4, BUN >70, and patient-reported functional decline. Difelikefalin’s FDA approval is a game-changer for uremic pruritus-targeting kappa opioid receptors without CNS depression. But don’t forget: optimal dialysis delivery is non-negotiable. No drug replaces inadequate clearance.
Oh please. They’re just pushing dialysis to make more money. You think they’d let you die if you didn’t pay? Nah-they’ll stick you in a chair for 4 hours a day, 3x a week, and bill your insurance $1,200 per session. Meanwhile, your kidneys are still there, just ‘failing’ by some arbitrary number. I’ve seen people survive on herbs and water fasting for years. This is corporate medicine.
Okay so I have stage 5 CKD and I’ve been itching like crazy for months-like, my husband says I scratch in my sleep-and I’ve been telling my doc but he just says ‘take antihistamines’ and ‘drink more water.’ Like… that’s not fixing the problem, dude. I finally got a referral to a nephrologist last week and they were like ‘holy crap why are you just now here?’ I’ve been losing weight, can’t eat meat, and my sleep score on my Apple Watch is lower than my ex’s dating profile. I started dialysis last Tuesday. First time I slept 7 hours straight. I cried. Not because I’m weak-because I forgot what it felt like to not be on fire.
Most of you are missing the point. This isn’t about medicine-it’s about societal neglect. In India, patients wait 8 months for dialysis because they can’t afford it. In the US, it’s about profit margins and bureaucratic inertia. The real uremia isn’t in the blood-it’s in the system that lets people suffer until they collapse. And no, gabapentin won’t fix that.
I’m so glad someone finally wrote this. My sister went through this. She thought it was just stress. She lost 20 pounds and stopped talking. When she finally got dialysis, she said, ‘I didn’t know I was this sick.’ Now she’s back to cooking for her grandkids. Please, if you’re feeling this-don’t wait. You’re not being strong. You’re just suffering in silence.
Y’ALL. I’m a nurse and I’ve seen this too many times. A woman came in last week with uremic pericarditis because she ‘didn’t want to be a burden.’ She was 52. She had a 10-year-old. She didn’t know she was dying. If you’re reading this and you’re having nausea or itching-CALL YOUR DOCTOR TODAY. Not tomorrow. TODAY. You don’t have to be ‘ready.’ Your body already is.
My dad’s been on dialysis for 5 years. He says the worst part wasn’t the needles-it was the itching. He used to sit in the dark just rubbing his arms. After starting Korsuva? He started gardening again. I didn’t think a pill could do that. But it did. This stuff matters.
Dialysis is a government scam. They’re poisoning you to keep you hooked. The toxins? Made up. The itching? Stress. They want you dependent. Look up ‘dialysis industry profits.’
From a clinical perspective: Kt/V >1.4 is the gold standard for hemodialysis adequacy. If you’re on peritoneal dialysis, aim for weekly Kt/V >1.7. For pruritus, serum phosphorus >5.5 mg/dL correlates strongly with severity. Gabapentin dosing must be adjusted-start at 100mg TID but monitor for sedation. Difelikefalin requires ECG monitoring due to QT risk. Always check renal drug clearance tables.
While the anecdotal evidence presented is compelling, the lack of longitudinal, randomized controlled trial data on symptom-based initiation renders this argument methodologically unsound. The IDEAL trial remains the most robust evidence to date. To prioritize patient-reported outcomes without standardized, validated instruments is to invite clinical chaos. One must not confuse sentiment with science.