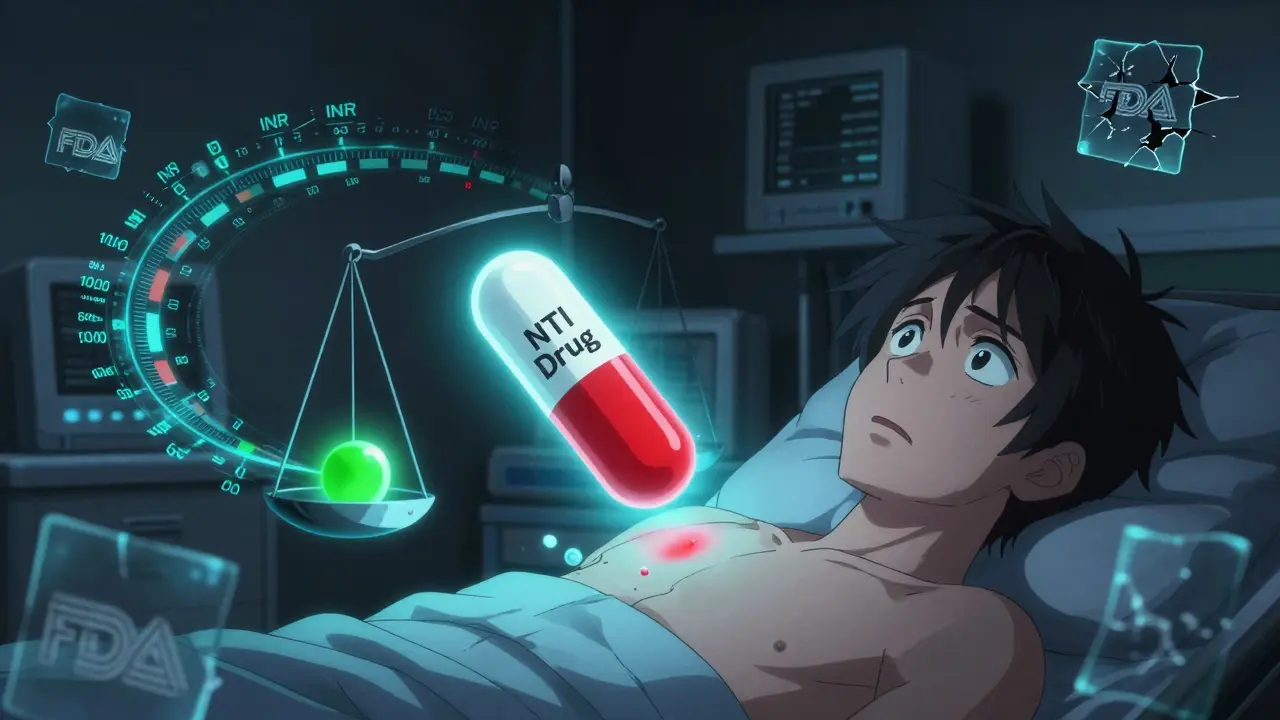
Studies show that switching to generic versions of NTI drugs like warfarin, phenytoin, and cyclosporine can lead to unstable blood levels, increased side effects, and serious health risks-even when generics are FDA-approved. What the data reveals about real-world outcomes.
NTI Drugs: What They Are, Why They Matter, and Which Medications Fall Into This Category
When a drug has a Narrow Therapeutic Index, a small difference between a safe dose and a toxic one. Also known as NTI drugs, these medications require extreme precision—too little won’t work, too much can land you in the hospital. Think of it like walking a tightrope: one wrong step and things go bad fast. This isn’t about side effects you can shrug off. With NTI drugs, even a 10% change in dose can trigger seizures, organ damage, or dangerous bleeding.
Common examples include warfarin, a blood thinner where tiny changes in dose can cause life-threatening clots or bleeds, phenytoin, an anti-seizure drug with a razor-thin safety margin, and levothyroxine, the thyroid hormone replacement where even slight fluctuations affect your heart, metabolism, and energy. These aren’t obscure drugs—they’re prescribed to millions. And because their levels in your blood are so sensitive to food, other meds, or even a change in manufacturer, monitoring isn’t optional. It’s mandatory.
That’s why switching from brand to generic, skipping a dose, or mixing them with certain supplements can be risky. You might not feel the difference right away, but your blood levels are shifting. That’s why doctors order regular blood tests for these drugs. That’s why pharmacists double-check prescriptions. And that’s why the posts here focus on real-world issues: how drug interactions, timing, and even your diet can make or break treatment. You’ll find guides on managing these meds safely, spotting hidden risks, and understanding why some drugs demand more attention than others. This isn’t theory. It’s about keeping you out of the ER and on track with your treatment.
NTI drugs like levothyroxine and phenytoin require strict dosing consistency. Insurers often require prior authorization for brand-name versions to prevent dangerous switches to generics. Learn why this policy exists - and how to get coverage.