Specialty Prescribing: Why Specialists Choose Brand-Name Drugs Over Generics

When a rheumatologist prescribes Humira instead of a biosimilar, or an oncologist insists on Ocrevus despite lower-cost alternatives, it’s not because they’re ignoring cost-it’s because they’ve seen what happens when patients switch. Specialty drugs aren’t just expensive. They’re complex, high-stakes treatments for conditions with few options. And when specialists choose brand-name drugs, it’s rarely about profit. It’s about survival.
The Reality of Specialty Drug Spending
Specialty drugs make up less than 2% of all prescriptions filled in the U.S., yet they account for over 70% of total pharmacy spending. In 2021, the average annual cost per patient on a specialty drug was $38,000. For non-specialty drugs? $492. That’s a 75-fold difference. These aren’t ordinary medications. They’re biologics, gene therapies, infusion-based treatments for cancers, multiple sclerosis, rheumatoid arthritis, and rare genetic disorders. Many require cold storage, trained nurses for administration, or daily injections. Some have narrow therapeutic windows-too little and the disease progresses; too much and you risk organ damage. The numbers don’t lie. Between 2010 and 2019, spending on specialty brand-name drugs jumped from $9.4 billion to $46.8 billion. By 2023, they made up 68% of all dispensing revenue from specialty drugs. And that growth isn’t slowing. Experts predict specialty drugs will consume 73% of global prescription drug spending by 2028.Why Generics Don’t Always Work
You’d think generics would be the obvious choice. They’re cheaper, approved by the FDA, and widely available. But for specialty drugs, the story is different. Many specialty drugs are biologics-complex proteins made from living cells. You can’t just copy them like you can a pill made of chemical compounds. What you get instead are biosimilars: drugs that are highly similar, but not identical. Here’s the catch: for some patients, even tiny differences matter. A 2023 Medscape survey found that 79% of rheumatologists say biosimilars aren’t appropriate for certain patients with autoimmune diseases. Why? Because switching can trigger a flare-up. One patient on Reddit shared that after switching from Humira to a biosimilar, her joint pain returned within weeks. Her rheumatologist told her: “Your body reacted to the original. We don’t risk changing it.” In oncology, the stakes are even higher. A single missed dose or delayed infusion can mean the difference between remission and progression. Specialists don’t gamble with treatments that have saved lives. They stick with what’s proven.Prescriber Pressure: It’s Not Just About Money
Some assume doctors choose brand-name drugs because they’re paid by pharmaceutical companies. There’s some truth to that. ProPublica’s 2016 analysis showed doctors who received over $5,000 from drugmakers prescribed brand-name drugs at rates 50% higher than those who received nothing. But that’s not the full picture. Most specialists aren’t swayed by free lunches or speaker fees. They’re swayed by data-and patient outcomes. A 2021 JAMA Network Open study found that prescribers and patients requested branded dispensing for 30.4% of multisource drugs. That’s $1.67 billion extra spent on Medicare, and $270 million out of patients’ pockets. But here’s the thing: many of those requests came from doctors who knew the alternative wouldn’t work. It’s also about liability. If a patient has a bad reaction after switching to a biosimilar, the doctor is on the hook. Insurance companies may push for cheaper options, but the doctor still has to answer for the outcome. That’s why many specialists refuse to switch patients unless there’s clear, published evidence of equivalence-and even then, they document every decision.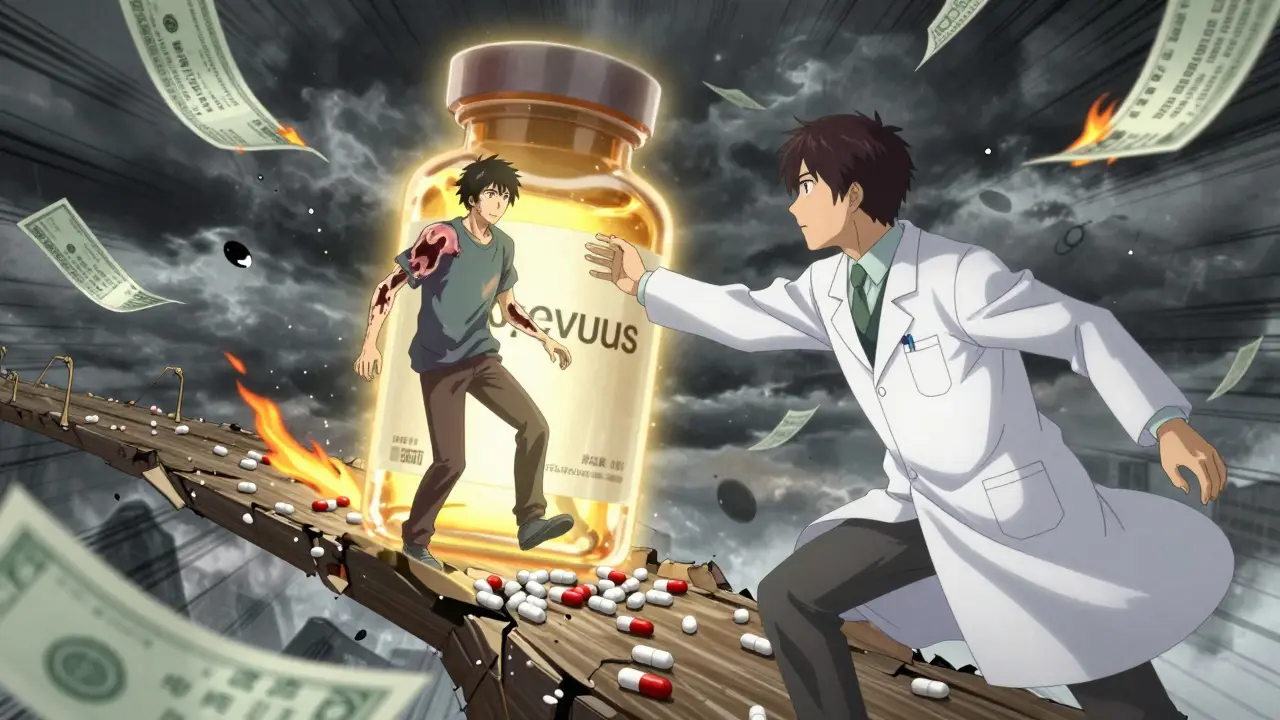
The Hidden System: PBMs and Markups
The real villain isn’t always the drugmaker. It’s the middlemen. Pharmacy Benefit Managers (PBMs)-Caremark, Express Scripts, OptumRx-control 68% of specialty drug dispensing. And they’re making massive profits on generics. The FTC’s January 2025 report found that PBMs marked up specialty generic drugs by thousands of percent. One drug bought for $100 was sold to patients for $15,000. That’s not a pricing error. That’s a business model. These markups don’t exist for traditional generics. Why? Because there’s competition. But for specialty drugs, PBMs own the pharmacies, control the formularies, and dictate what doctors can prescribe. Doctors don’t set these prices. They’re stuck in a system where the cheapest option isn’t always the most affordable for the patient. A patient might have a $50 copay on a brand-name drug because their plan has a tiered structure. Switch to the “generic,” and suddenly their copay jumps to $850 because the PBM’s markup is so high.Administrative Nightmares
Even when a specialist wants to prescribe a generic, the system gets in the way. Prior authorization forms take hours to complete. Insurance companies demand lab results, failed trial records, and signed consent forms. A 2024 study found that 42% of specialty drug starts are delayed by seven or more days because of paperwork. Physicians spend an average of 13.4 hours per week on prior authorizations-78% of that time tied to specialty drugs. That’s not time spent diagnosing. That’s time spent fighting insurance. And it’s not just the doctor. Patients are drowning in bureaucracy. One Medicare enrollee wrote on a patient forum: “My Humira copay went from $50 to $850 when my plan changed. My doctor says the biosimilar won’t work for me. But my insurer won’t cover the brand unless I appeal. I’ve been waiting six weeks.”
What’s Changing?
There’s pressure to fix this. The Inflation Reduction Act of 2022 let Medicare negotiate prices for some high-cost drugs. Starting in 2026, drugs like Jakafi, Ofev, and Xtandi could be subject to price caps. The FTC is investigating PBM markups. Senator Bernie Sanders introduced the Specialty Drug Price Transparency Act in February 2025 to force PBMs to disclose their pricing practices. But change is slow. And for now, specialists are still making decisions based on one question: “Will this save my patient’s life-or just their wallet?”What Patients Should Know
If your specialist insists on a brand-name drug, don’t assume they’re being paid off. Ask: “Is there a proven alternative? What happens if I switch?” Get the data. Ask for studies. Ask if the alternative has been tested in patients like you. If your insurance denies coverage, appeal. Document everything. Reach out to patient advocacy groups like NORD or the Arthritis Foundation-they help thousands get access to specialty drugs every year. And remember: the system is broken. But your doctor isn’t the problem. They’re trying to navigate it with your life on the line.Why don’t specialists just switch to cheaper generics?
Many specialty drugs are biologics, which don’t have true generics-only biosimilars. These are similar, but not identical. For some patients, switching can cause disease flares, reduced effectiveness, or dangerous side effects. Specialists avoid switching unless there’s strong clinical evidence that the alternative works just as well for that specific patient.
Are doctors paid to prescribe brand-name drugs?
Sometimes, yes. Studies show doctors who receive payments from drug companies prescribe brand-name drugs more often. But most specialists choose brand-name drugs because they’ve seen what happens when patients switch to alternatives that don’t work. Their decisions are based on outcomes, not kickbacks.
Why are specialty drugs so expensive?
Specialty drugs are complex to develop, require special handling, and treat rare or life-threatening conditions with few alternatives. Drugmakers set high prices because they know patients have no other options. Pharmacy Benefit Managers (PBMs) then add massive markups-sometimes thousands of percent-on what are supposed to be cheaper generic versions.
Can I ask my doctor for a biosimilar instead?
Yes, absolutely. But ask for the reasoning behind their recommendation. Request studies or data showing how the biosimilar compares for your specific condition. Some patients respond well. Others don’t. Your doctor should be able to explain why one is better for you.
What if my insurance won’t cover the brand-name drug?
Appeal the denial. Ask your doctor to write a letter of medical necessity. Contact patient assistance programs from organizations like NORD or the manufacturer. Many drugmakers offer co-pay assistance or free drug programs for eligible patients. Don’t give up-these programs help tens of thousands each year.
Is there any hope for lower prices in the future?
Yes. The Inflation Reduction Act allows Medicare to negotiate prices for some specialty drugs starting in 2026. New laws are being proposed to force PBMs to disclose markups. But change moves slowly. Until then, patients and doctors are stuck in a system designed to maximize profits, not health.



Been there. My mom switched to a biosimilar for her RA and it was a nightmare. Pain came back harder than before. Doctor said no more swaps. I get why they stick with the brand.
Not about money. About not watching someone suffer because of a cost-cutting loophole.
Oh wow. So doctors are saints now? The system is broken but *they* are blameless? Cute. Tell that to the patient who had to sell their car to afford Humira because their PBM marked up the ‘generic’ to $12k. You think this is about survival? It’s about inertia wrapped in a white coat.
My cousin is on Ocrevus and she’s been stable for 4 years. They tried the biosimilar once and she ended up in the hospital. Doctor didn’t even hesitate after that. He said ‘I’m not risking her life for a 10% savings’.
That’s the real talk right there. No fluff. Just facts. And patients deserve that kind of loyalty.
YES THIS!! 🙌
Doctors aren’t the villains here. The system is. PBMs are literally gouging people and calling it ‘generic’. I cried reading that $100 → $15,000 stat. Someone needs to burn this whole thing down and start over. ❤️
It’s funny how we frame this as a moral dilemma between profit and life. But what if the real question is: why does a society that claims to value life also build systems that make healing a lottery?
Specialists aren’t heroes. They’re just the last line of defense in a broken machine. And we keep asking them to hold the dam with their bare hands.
Of course the doctors choose the brand. They don’t want to be sued. They don’t want to lose sleep. They don’t care if you go bankrupt. They just want to check the box and move on. Don’t romanticize them. They’re just playing the game.
Let’s be clear: the problem isn’t that doctors choose brand-name drugs-it’s that the system forces them to choose between ethical care and administrative survival. Prior auth forms take longer than actual patient visits. PBMs control formularies like monopolies. And patients? They’re collateral damage in a profit-driven game disguised as healthcare.
Fix the middlemen. Not the messengers.
Everyone’s mad at the doctors but no one’s mad at the PBMs. That’s the real story here. Why? Because it’s easier to blame the person holding the pen than the person who wrote the whole damn rulebook.
Doctors are stuck between a rock and a hard place. We need to fix the system-not shame the people trying to survive inside it.
Oh so the American doctor is the knight in shining armor while the PBM is the dragon? How poetic. In India, we don’t have this luxury. We use generics because we have to. And guess what? Most patients do just fine.
Maybe your ‘life-saving’ drugs are just overpriced placebo with a fancy label? Maybe your system is the disease?
The data is clear: biosimilars are statistically non-inferior in 90% of cases. The remaining 10%? That’s where clinical judgment matters. But the fact that 79% of rheumatologists refuse *any* switch suggests confirmation bias, not clinical necessity. Where are the longitudinal studies? Where’s the transparency? Until then, this is fear, not science.
My uncle’s on a specialty drug. He pays $40 a month for the brand. Switched to the ‘generic’ once. Copay jumped to $1100. His insurance didn’t even tell him. He found out when the pharmacy refused to fill it.
It’s not about the drug. It’s about the game.
The system is rigged and no one wants to admit it
Wait so if the PBM is making $15k off a $100 drug, who’s actually profiting? The drugmaker? Or the middleman who doesn’t even make the medicine?
And why do we still call it a ‘generic’ when it’s 150x the cost? That’s not a drug. That’s a scam with a pharmacy logo.
Also, my doctor told me the same thing about Humira. Said switching was like changing your car engine mid-drive. I believed him. But now I’m wondering… if the system were fair, would he even have to say that?