How Verapamil Can Help with the Management of Chronic Pain

Most people think of verapamil as a heart medication-something you take for high blood pressure or an irregular heartbeat. But if you’ve been living with chronic pain for years, especially nerve-related pain, you might not know that verapamil is being used off-label to help calm down stubborn pain signals. It’s not a first-line treatment, but for some people, it’s the missing piece they didn’t know they needed.
What verapamil actually does in the body
Verapamil is a calcium channel blocker. That means it stops calcium from entering certain cells, especially in the heart and blood vessels. Less calcium means relaxed blood vessels, lower blood pressure, and slower heart rate. But calcium doesn’t just affect the heart-it’s also a key player in how nerve cells communicate.
In chronic pain, especially neuropathic pain, nerves become overactive. They fire too often, too easily, or even when there’s no injury. This isn’t just "bad nerves." It’s a biological glitch where calcium floods into nerve endings, triggering excessive release of pain-signaling chemicals like glutamate and substance P. Verapamil, by blocking calcium channels in these nerves, can reduce that over-firing. It doesn’t numb you. It doesn’t make you sleepy. It just quiets the noise.
Who benefits most from verapamil for pain?
Verapamil isn’t a magic bullet for all chronic pain. It’s most helpful for conditions where nerve irritation or abnormal signaling is the main driver. These include:
- Trigeminal neuralgia-sharp, electric shock-like facial pain that comes and goes. Some patients report fewer attacks after starting verapamil, even when carbamazepine stopped working.
- Complex regional pain syndrome (CRPS)-a painful condition often following injury, where the nervous system goes haywire. Studies show verapamil can reduce swelling, burning pain, and skin changes in some cases.
- Chronic cluster headaches-not just bad headaches, but excruciating, recurring pain around one eye. Verapamil is actually a standard preventive treatment here, even though it’s not a painkiller.
- Diabetic neuropathy-some patients with burning, tingling feet report modest improvement when other meds like gabapentin or duloxetine don’t cut it.
It’s not for osteoarthritis, back pain from disc issues, or muscle spasms. Those need different approaches. Verapamil targets nerve hyperexcitability. If your pain feels like a fire alarm stuck on, this might help. If it’s a sore joint, it won’t.
How it compares to other pain meds
Most chronic pain treatments fall into a few buckets: anti-inflammatories, antidepressants, anticonvulsants, or opioids. Verapamil sits outside those groups.
| Medication | Primary Use | Common Side Effects | Works for Nerve Pain? | Dependence Risk |
|---|---|---|---|---|
| Verapamil | Calcium channel blocker | Constipation, dizziness, low blood pressure | Yes, for specific types | Very low |
| Gabapentin | Anticonvulsant | Drowsiness, dizziness, weight gain | Yes | Low |
| Duloxetine | Antidepressant (SNRI) | Nausea, dry mouth, insomnia | Yes | Low |
| Morphine | Opioid | Constipation, nausea, tolerance, addiction | Moderate | High |
| Corticosteroids | Anti-inflammatory | Bone loss, high blood sugar, mood swings | No | None |
Verapamil’s biggest advantage? It doesn’t cause dependence or tolerance. You won’t need higher doses over time just to get the same effect. It also doesn’t cloud your thinking like some anticonvulsants do. The trade-off? It can lower your blood pressure too much, especially if you’re already on other meds. That’s why you need medical supervision.
How it’s prescribed for pain
Doctors don’t just hand out verapamil for pain. It’s always off-label-meaning it’s not officially approved for pain by regulators like the FDA or TGA. But that doesn’t mean it’s experimental. It’s based on clinical experience and peer-reviewed studies.
Typical starting doses for pain range from 40 mg to 80 mg once or twice daily. Some patients go up to 240 mg per day, split into doses. It takes time-often 2 to 6 weeks-to see if it helps. You can’t expect overnight relief. The goal isn’t to eliminate pain completely, but to reduce it enough that you can sleep, move, or do daily tasks without being overwhelmed.
It’s usually tried after first-line nerve pain meds fail. If gabapentin gave you brain fog and duloxetine made you nauseous, verapamil might be the next logical step. Some doctors combine it with low-dose nortriptyline or topical lidocaine for layered relief.
What to watch out for
Verapamil is generally safe-but not for everyone. You should avoid it if you have:
- Heart failure with low blood pressure
- Second- or third-degree heart block (without a pacemaker)
- Severe liver disease
- Are already taking beta-blockers like metoprolol
Common side effects include constipation (which can be managed with fiber and water), dizziness when standing up, and mild swelling in the ankles. Rarely, it can cause slow heart rate or liver enzyme changes. That’s why blood pressure and heart rate are checked regularly, and liver tests may be done after a few months.
It also interacts with many common drugs: statins, certain antibiotics like clarithromycin, and even grapefruit juice. Grapefruit can spike verapamil levels in your blood, raising the risk of side effects. Always tell your doctor or pharmacist what else you’re taking.

Real stories: When verapamil made a difference
One patient in her late 50s had trigeminal neuralgia for 8 years. She’d tried carbamazepine, oxcarbazepine, and even a nerve block. Nothing lasted. She started verapamil at 80 mg daily. After three weeks, her pain attacks dropped from 15 a day to 2 or 3. She stopped wearing a face scarf everywhere. She started gardening again.
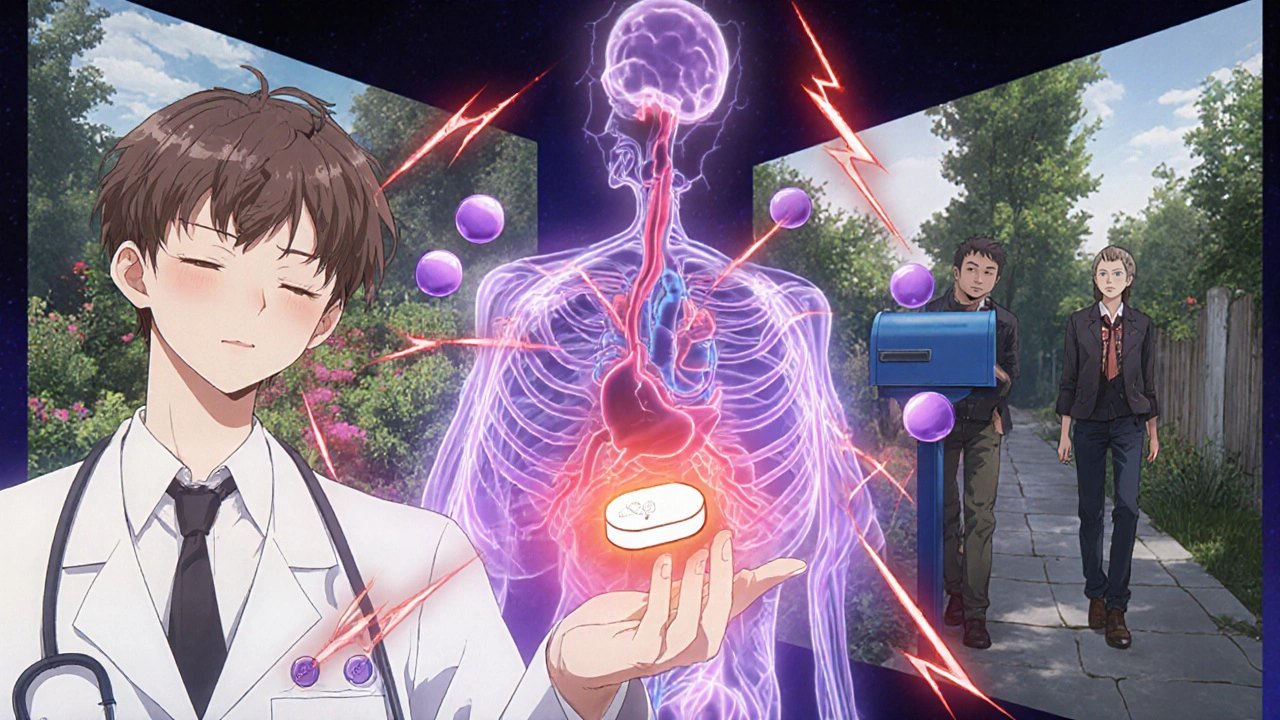
A man in his 40s developed CRPS after a minor ankle sprain. His foot burned constantly. He couldn’t wear shoes. Gabapentin helped a little, but he felt drugged. After adding verapamil 120 mg daily, his burning eased by about 60%. He could walk to the mailbox again. He didn’t feel numb-he just didn’t hurt as much.
These aren’t outliers. They’re people who found relief where other options failed. Verapamil isn’t glamorous. It’s not new. But for chronic nerve pain, it’s quietly effective for a subset of patients who’ve run out of choices.
Is verapamil right for you?
If you’ve been on multiple pain meds with little success, and your pain feels like nerves firing out of control, ask your doctor about verapamil. Bring up the specific condition you have. Ask if your pain pattern matches those studied in clinical reports.
Don’t expect miracles. Don’t self-prescribe. But don’t dismiss it either. Many doctors don’t mention it because they’re trained to think of it as a heart drug. But pain specialists know better. In Melbourne, at the Royal Melbourne Hospital’s pain clinic, verapamil is part of the toolkit for patients who haven’t responded to standard treatments.
It’s not the first thing you try. But it might be the one that finally gives you back some peace.
Can verapamil be used for everyday headaches?
No, verapamil isn’t meant for typical tension headaches or migraines unless they’re cluster headaches. Cluster headaches are a rare, severe type that happen in cycles, often around one eye. Verapamil is actually a standard preventive for this specific condition. For regular migraines or tension headaches, other medications like beta-blockers, topiramate, or even triptans are more appropriate.
How long does it take for verapamil to work for pain?
It usually takes 2 to 6 weeks to see any effect. Unlike painkillers that work in minutes, verapamil works by gradually calming overactive nerves. You won’t feel relief right away. Patience is key. If there’s no improvement after 8 weeks, it’s unlikely to help, and your doctor may consider switching options.
Is verapamil addictive?
No, verapamil is not addictive. It doesn’t affect the brain’s reward system like opioids or even some anti-anxiety drugs. You won’t crave it, and you won’t need to increase the dose over time to get the same effect. However, stopping it suddenly can cause rebound high blood pressure or worsening of heart rhythm issues, so always taper under medical supervision.
Can I take verapamil with other pain meds?
Yes, but carefully. Verapamil is often combined with gabapentin, low-dose antidepressants like nortriptyline, or topical treatments like lidocaine patches. But it can interact with NSAIDs, statins, and some antibiotics. Always tell your doctor and pharmacist about every medication and supplement you’re taking-including herbal ones like St. John’s wort or garlic pills.
Does verapamil help with inflammation?
Not directly. Verapamil doesn’t reduce swelling or inflammation like ibuprofen or corticosteroids. Its pain-relieving effect comes from calming overactive nerves, not from fighting inflammation. So if your pain is from arthritis or tendonitis, verapamil won’t help much. It’s best for nerve-based pain, not tissue-based pain.
If you’ve tried everything else and your pain still won’t quit, verapamil might be worth a conversation with your doctor. It’s not flashy, but for the right person, it’s a quiet game-changer.


verapamil for pain?? lmao so now theyre just repurposing heart pills like its some kind of miracle drug? i bet the pharma companies love this-same pill, new label, same profit. next theyll tell us tylenol cures depression. i’ve seen people on this stuff get so dizzy they fall down stairs. dont believe the hype.
oh sure, let’s just ignore the fact that verapamil was originally developed by a german pharmaceutical giant with ties to the military-industrial complex. why do you think they’re pushing it for nerve pain? it’s not about relief-it’s about controlling the nervous system. they want us docile. ask yourself: who benefits when millions are quietly sedated with calcium blockers instead of addressing trauma, pollution, or glyphosate in our food?
While the off-label use of verapamil for neuropathic pain is supported by a modest body of clinical literature, it is imperative to emphasize that its efficacy is highly condition-specific. The pharmacodynamic profile of verapamil as a non-dihydropyridine calcium channel blocker does indeed modulate neuronal excitability, particularly in voltage-gated calcium channels of type L, which are implicated in the pathophysiology of trigeminal neuralgia and cluster headaches. However, the absence of large-scale randomized controlled trials limits its recommendation to second- or third-line therapy in most clinical guidelines. Caution is warranted in patients with preexisting conduction abnormalities or concurrent beta-blocker use due to additive negative chronotropic effects.
HAHAHA you westerners think you invented medicine? in india, we’ve been using natural calcium regulators like ashwagandha and turmeric for 5000 years to calm nerves. now you’re giving people heart pills because your doctors are too lazy to learn real healing? you people take 12 pills a day and still cry about pain. we don’t need your verapamil-we need to stop eating processed sugar and sitting on chairs all day. your whole system is broken. your medicine is a scam. we knew this before you even had a word for "neuropathy".
The assertion that verapamil constitutes a viable therapeutic alternative for neuropathic pain lacks sufficient empirical validation under the current standards of evidence-based medicine. Although anecdotal case reports exist, the absence of FDA approval for this indication, coupled with the potential for clinically significant hypotension and bradycardia, renders its use in this context both inappropriate and potentially hazardous without rigorous patient selection and monitoring. Furthermore, the proliferation of off-label prescriptions contributes to the erosion of pharmaceutical regulatory integrity.
i tried verapamil for 6 weeks after my fibro flared. i felt like a zombie with constipation and zero energy. my doctor said "give it time." time for what? to turn into a human raisin? i stopped it. now i take cbd oil and cry into my pillow. at least that doesn’t make me feel like my insides are made of concrete. why do doctors keep pushing stuff that just makes you sadder and slower?
It’s worth noting that verapamil’s mechanism in neuropathic pain is not fully understood but is likely tied to its ability to inhibit presynaptic calcium influx, thereby reducing the release of excitatory neurotransmitters like glutamate and substance P in the dorsal horn of the spinal cord and peripheral nerve terminals. This is distinct from gabapentin’s action on the α2δ subunit of voltage-gated calcium channels. Clinical trials, such as the 2018 randomized study in *Neurology* involving 67 patients with refractory trigeminal neuralgia, showed a 40% reduction in attack frequency compared to placebo. Dosing should be titrated slowly-starting at 40 mg BID-and blood pressure should be monitored twice weekly during the first month. Patients with hepatic impairment require dose adjustments, and grapefruit juice must be strictly avoided due to CYP3A4 inhibition. Long-term use appears safe in compliant patients without contraindications, and unlike opioids, there is no tolerance development or withdrawal syndrome. For the right patient, this is a quiet but powerful tool.
Verapamil’s utility in CRPS and trigeminal neuralgia is well-documented in neuropharmacological literature. The key lies in targeting T-type and L-type calcium channels in hyperexcitable nociceptors. However, most clinicians lack the requisite neurophysiological literacy to implement this appropriately. They prescribe it as a last-ditch effort rather than a precision tool. You need a pain specialist who understands channelopathies-not a GP who thinks it’s just another antihypertensive. Also, co-administration with SNRIs requires caution due to additive QT prolongation risk. If you’re not monitoring ECG and serum levels, you’re not treating-you’re gambling.