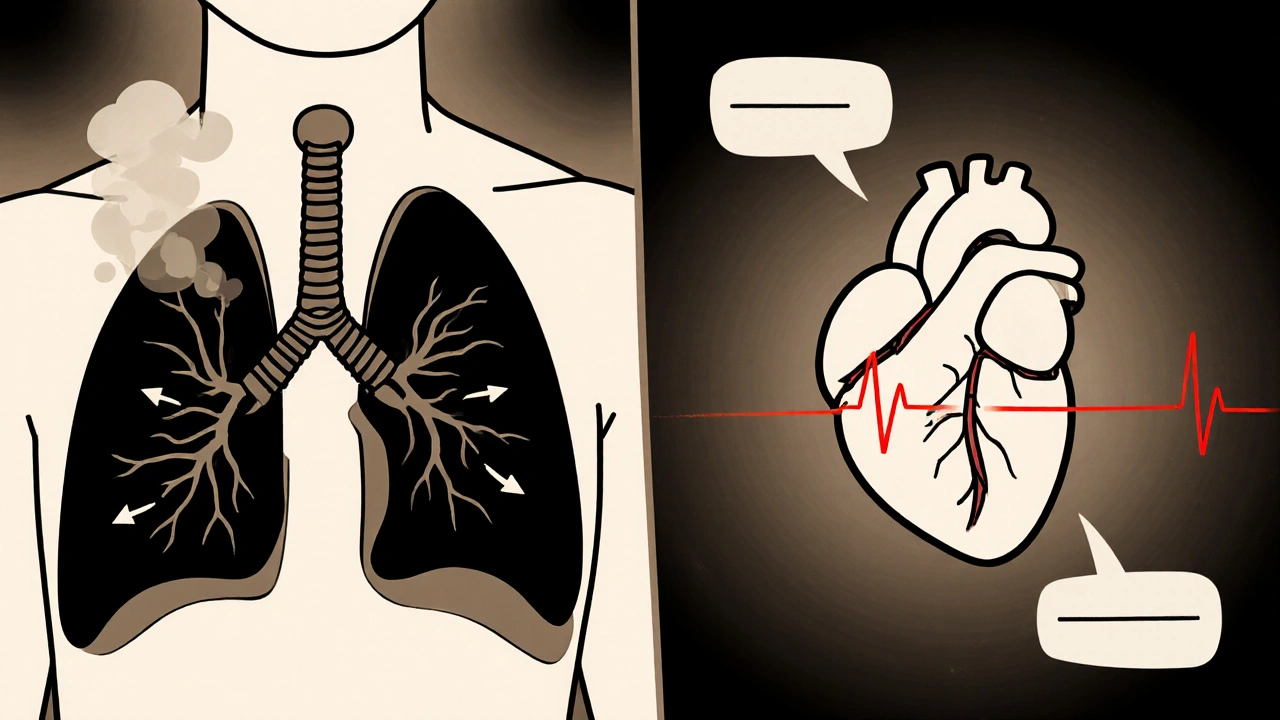
Explore how obstructive pulmonary disease (COPD) strains the heart, triggers pulmonary hypertension, and accelerates atherosclerosis, plus practical steps to lower cardiovascular risk.
Systemic Inflammation: What It Is and Why It Matters
When dealing with systemic inflammation, a whole‑body inflammatory response that can drive chronic disease. Also known as chronic inflammation, it affects organs, blood vessels, and metabolism all at once. A key driver is the cytokine storm, an explosive release of signaling proteins that amplify immune activity, which often follows infections or severe stress. The gut microbiome, the community of bacteria living in our intestines can either calm or fuel this response, making diet and probiotic use critical. Likewise, autoimmune disorders, conditions where the immune system attacks healthy tissue constantly trigger low‑grade systemic inflammation. In short, systemic inflammation connects cytokine storms, gut health, and autoimmunity in a three‑way loop.
One major consequence of this loop is damage to the cardiovascular system. When inflammatory markers like C‑reactive protein rise, blood vessels become sticky, raising blood pressure and paving the way for heart disease. Medications such as ACE inhibitors (e.g., Capoten) and statins not only lower cholesterol but also blunt inflammatory pathways, showing how drug choice can directly impact systemic inflammation. Oxidative stress—an excess of free radicals—works hand‑in‑hand with inflammation, each feeding the other and accelerating tissue aging. Vitamin K deficiency, for example, worsens clotting problems and bone health, both of which are sensitive to inflammatory status. Understanding these links helps you see why managing inflammation is a cornerstone of heart and bone protection.
Lifestyle Levers That Tame Systemic Inflammation
Everyday habits shape the inflammatory landscape. Regular aerobic exercise boosts anti‑inflammatory cytokines and improves insulin sensitivity, which keeps the immune system from overreacting. Stress‑reduction techniques like yoga and meditation lower cortisol, a hormone that can trigger cytokine release when chronically high. Nutrition plays a starring role: diets rich in antioxidants, omega‑3 fatty acids, and fiber nurture a balanced gut microbiome, while excess caffeine or processed sugars can tip the scales toward inflammation and even raise osteoporosis risk. Probiotic‑rich foods such as kefir or sauerkraut introduce beneficial microbes that compete with harmful strains, reducing gut‑derived inflammatory signals that travel through the bloodstream.
From a clinical standpoint, tracking inflammation is easier than you think. Simple blood tests for C‑reactive protein (CRP) or erythrocyte sedimentation rate (ESR) give a snapshot of systemic activity. When these numbers climb, doctors may recommend lifestyle tweaks first, then consider anti‑inflammatory medications like low‑dose aspirin or specific disease‑modifying agents for autoimmune patients. The choice of drug often hinges on the underlying cause: ACE inhibitors are favored for hypertension‑related inflammation, while biologics target cytokine storms in severe autoimmune flare‑ups. Knowing which pathway dominates allows a more precise, less risky approach.
Putting all these pieces together, you can view systemic inflammation as a hub where diet, gut health, stress, and medication intersect. Whether you’re battling high blood pressure, managing an autoimmune condition, or simply looking to protect your bones, reducing chronic inflammation offers a unifying strategy. The articles below dive deeper into each angle—blood‑pressure meds vs. alternatives, the impact of caffeine on bone loss, how yoga calms psoriasis, and more. Browse the collection to find practical tips, drug comparisons, and science‑backed guidance that fit your situation.