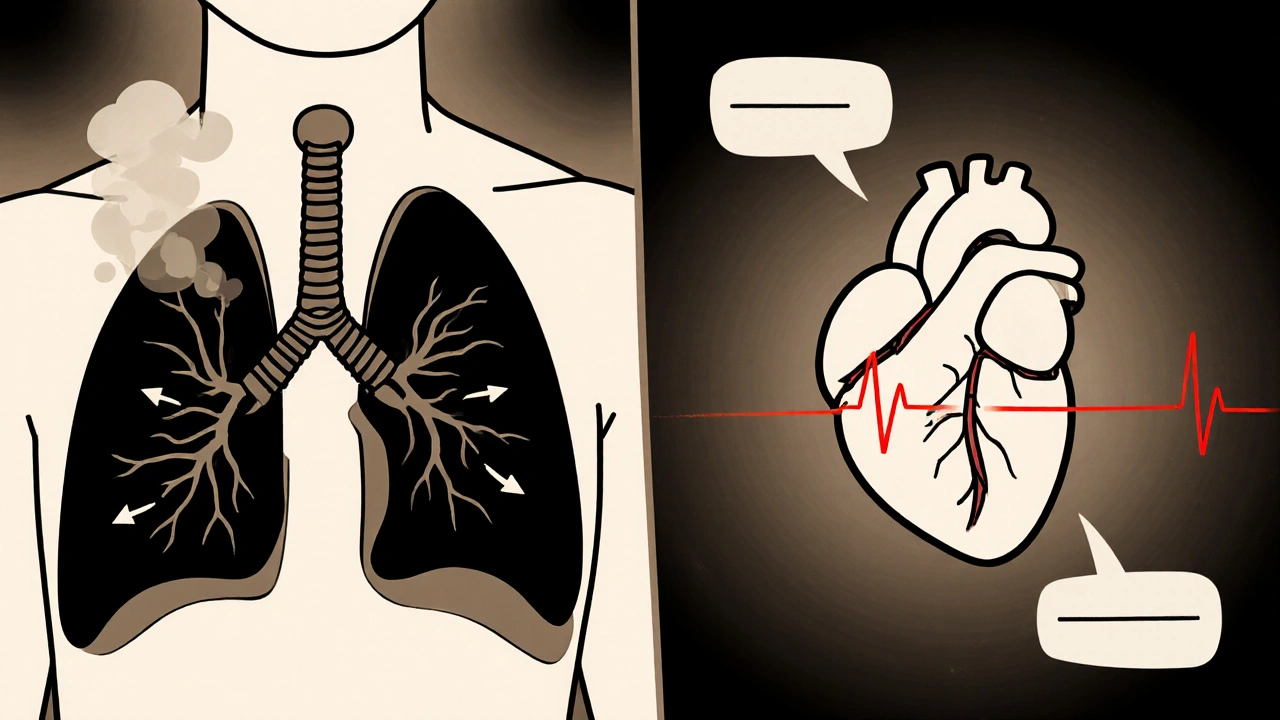
Explore how obstructive pulmonary disease (COPD) strains the heart, triggers pulmonary hypertension, and accelerates atherosclerosis, plus practical steps to lower cardiovascular risk.
Pulmonary Hypertension: Causes, Symptoms, and Treatment Options
When dealing with pulmonary hypertension, a condition where the blood pressure in the lung arteries climbs far above normal. Also known as high pulmonary arterial pressure, it forces the right side of the heart to work harder, can cause breathlessness, fatigue, and may lead to serious heart complications if left unchecked. The core problem is an increase in vascular resistance inside the lungs, which means the heart must pump against a tougher road. People often confuse it with systemic high blood pressure, but the two systems are separate; pulmonary hypertension specifically targets the lungs and the right ventricle.
Key Treatment Options and Related Concepts
One of the first drug families doctors reach for are ACE inhibitors, medications that relax blood vessels by blocking the conversion of angiotensin I to angiotensin II. They lower systemic pressure and, in some cases, ease the load on the pulmonary circulation, especially when left‑heart disease contributes to the problem. The recent comparison of Capoten (captopril) with newer blood‑pressure agents shows how a classic ACE inhibitor can still hold its own in safety and kidney protection, which matters for patients already dealing with compromised heart function. Another powerful class is endothelin receptor antagonists, drugs that block endothelin‑1, a molecule that makes lung vessels constrict. By preventing this tightening, they directly target the root cause of high pulmonary pressure. Examples like bosentan and ambrisentan have become staples in modern treatment plans, often combined with other vasodilators for a multi‑hit approach. For patients with advanced disease, prostacyclin therapy, infusions or inhaled agents that mimic a natural vessel‑relaxing substance offers a lifeline. Prostacyclins widen the pulmonary arteries, improve oxygen exchange, and can even reverse some vascular remodeling. The trade‑off is more complex administration—continuous IV pumps or inhalers—but the benefits in exercise capacity and survival are well documented. All these therapies aim to prevent or delay right heart failure, a condition where the right ventricle cannot keep up with the pressure load from the lungs. When the right ventricle weakens, symptoms jump from mild shortness of breath to swelling in the legs, fainting episodes, and severe fatigue. Monitoring right‑ventricular function with echo or MRI becomes a crucial part of managing pulmonary hypertension, guiding medication adjustments and timing for advanced interventions. Together, these drug classes create a layered treatment strategy: ACE inhibitors for systemic support, endothelin antagonists for targeted vessel relaxation, and prostacyclins for direct pulmonary vasodilation. Each has its own profile of side effects, dosing considerations, and cost factors, which is why personalized care plans are essential.
Below you’ll find a curated set of articles that dive deeper into the medicines and health issues surrounding this condition. From a side‑by‑side look at Capoten versus newer ACE inhibitors, to insights on how common drugs like mefloquine or ziprasidone intersect with cardiovascular health, the collection offers practical guidance you can apply right away. Whether you’re a patient trying to understand your prescription, a caregiver seeking clear explanations, or a health‑professional looking for up‑to‑date comparisons, the posts ahead cover the full spectrum of treatment decisions, lifestyle impacts, and emerging research related to pulmonary hypertension.