Steroid-induced psychosis is a dangerous but treatable side effect of high-dose corticosteroids. Learn how to recognize early signs, rule out mimics, and manage it safely in an emergency with tapering and low-dose antipsychotics.
Emergency Management of Psychosis
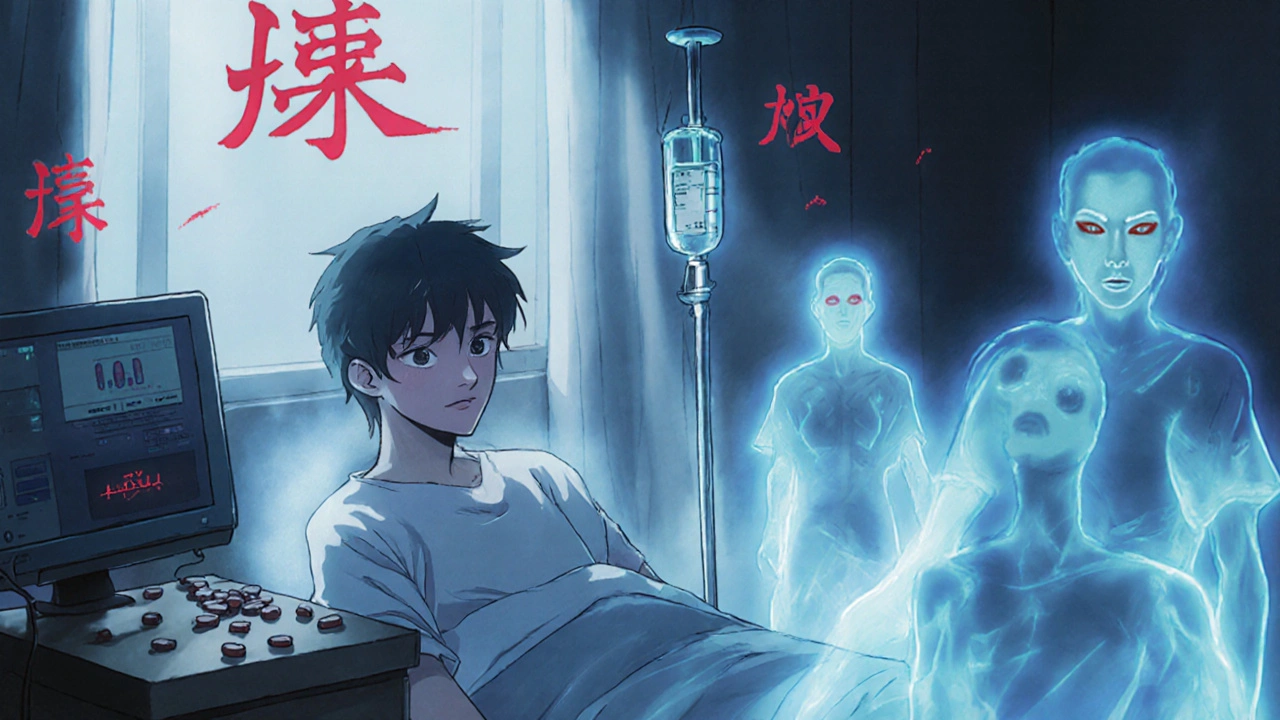
When someone is in the middle of a psychotic episode, a sudden loss of contact with reality marked by hallucinations, delusions, or extreme disorganization. Also known as acute psychosis, it requires immediate intervention to prevent harm to the person or others. This isn’t a slow-burn issue—it’s a crisis that unfolds in minutes, not days. Emergency teams don’t wait for perfect diagnoses. They act on symptoms: loud shouting, paranoia, aggression, or catatonia. The goal? Calm the person down, keep everyone safe, and start treatment fast.
Two types of drugs are the backbone of emergency management: antipsychotics, medications that block dopamine in the brain to reduce hallucinations and delusions and benzodiazepines, sedatives that calm agitation and anxiety quickly. For antipsychotics, injectable forms like haloperidol or olanzapine are common because they work in 15 to 30 minutes. Benzodiazepines like lorazepam or midazolam kick in even faster—sometimes in under 10 minutes. Together, they’re a powerful combo. You don’t need to pick one; you use both when someone is screaming, swinging, or terrified. The key is speed, not perfection.
What you don’t do matters just as much as what you do. Avoid forcing oral meds on someone who won’t swallow—they’ll spit them out or choke. Don’t try to reason with delusions. Saying "That’s not real" just makes them more scared. And never ignore the body. High fever, stiff muscles, or rapid heartbeat could mean neuroleptic malignant syndrome—a rare but deadly side effect of antipsychotics. Emergency staff check vitals constantly. They also look for triggers: drug use, missed meds, infections, or metabolic problems. A simple blood test can reveal if low sodium or a thyroid crash is causing the psychosis, not schizophrenia.
Most people who have a psychotic break don’t have schizophrenia. It could be bipolar disorder, a reaction to stimulants like meth or cocaine, or even a severe vitamin deficiency. Emergency care isn’t about labeling—it’s about stabilizing. Once the person is calm, doctors start digging deeper. But in the moment? It’s about safety, speed, and stopping the storm. That’s why the best emergency teams carry both antipsychotics and benzodiazepines in their kits—they know the clock is ticking.
What you’ll find in the posts below isn’t theory—it’s real-world insight. You’ll see how ziprasidone affects long-term mental health, why certain drugs like carbamazepine can trigger dangerous skin reactions, and how antipsychotics interact with heart conditions. You’ll also learn about patient advocacy, insurance hurdles, and how to avoid dangerous drug combinations. This isn’t a textbook. It’s a practical guide for people who need answers fast—whether you’re a patient, a caregiver, or just trying to understand what happens when someone loses touch with reality.