Steroid-induced psychosis is a dangerous but treatable side effect of high-dose corticosteroids. Learn how to recognize early signs, rule out mimics, and manage it safely in an emergency with tapering and low-dose antipsychotics.
Corticosteroid Psychosis: Causes, Risks, and What You Need to Know
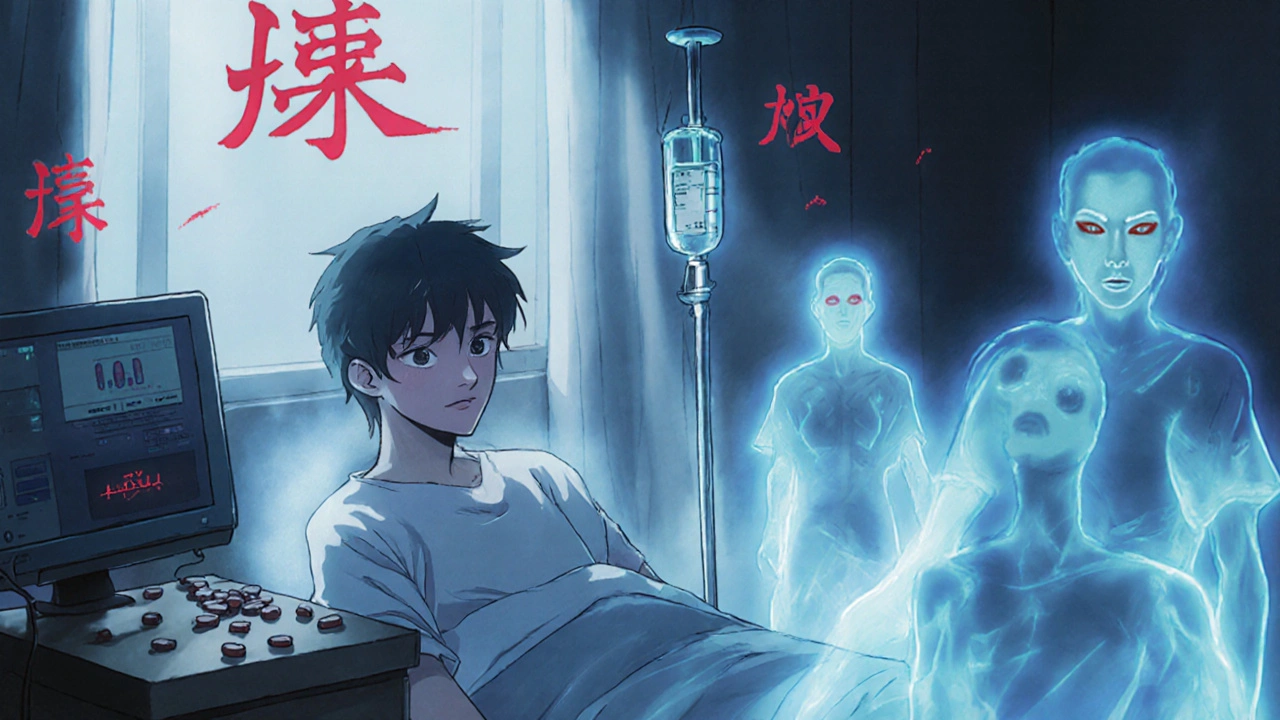
When you take corticosteroid psychosis, a psychiatric condition triggered by corticosteroid medications that causes hallucinations, delusions, or severe mood swings. It's not rare—it happens in up to 6% of people on high-dose steroids, especially those with pre-existing mental health conditions or taking them for long periods. This isn’t just "feeling jittery" or being moody. It’s a full-blown break from reality that can land someone in the hospital.
corticosteroids, powerful anti-inflammatory drugs like prednisone, dexamethasone, and methylprednisolone used for asthma, lupus, and autoimmune diseases are lifesavers for many. But they don’t just calm inflammation—they also flood your brain with synthetic cortisol, messing with neurotransmitters like serotonin and dopamine. That’s why steroid-induced psychosis, a subtype of corticosteroid psychosis that appears suddenly after starting or increasing steroid doses often hits within days or weeks. People report hearing voices, believing they’re being watched, or feeling paranoid without reason. Some get manic. Others sink into deep depression. The symptoms can be terrifying—and they’re often mistaken for schizophrenia or bipolar disorder.
It’s not just about the dose. Genetics matter. So does age—older adults and those with prior mental illness are at higher risk. Even short bursts of high-dose steroids, like during a flare-up, can trigger this. And here’s the catch: doctors don’t always connect the dots. Patients are told they’re "just stressed" or "anxious," when what they’re experiencing is a direct drug reaction. The good news? It usually goes away once the steroid is tapered down, but only if it’s recognized early. Waiting too long can lead to longer recovery or even permanent changes in brain chemistry.
If you’re on steroids and start feeling off—like your thoughts are racing, you’re seeing things that aren’t there, or you’re convinced someone is out to get you—don’t ignore it. Tell your doctor immediately. Don’t wait. Don’t assume it’s "all in your head." This is a biological reaction to a chemical, not a personal failure. And if you’re caring for someone on long-term steroids, watch for changes in behavior. A sudden shift in personality, sleeplessness, or irrational anger could be a red flag.
Below, you’ll find real stories and clinical breakdowns from people who’ve lived through this. Some found relief after switching medications. Others needed antipsychotics temporarily. A few didn’t get help fast enough—and paid the price. These aren’t hypotheticals. They’re real cases, with real outcomes. What you read here could help you or someone you love avoid a crisis.