Steroid-induced psychosis is a dangerous but treatable side effect of high-dose corticosteroids. Learn how to recognize early signs, rule out mimics, and manage it safely in an emergency with tapering and low-dose antipsychotics.
Antipsychotics for Steroid Psychosis: What Works and What to Watch
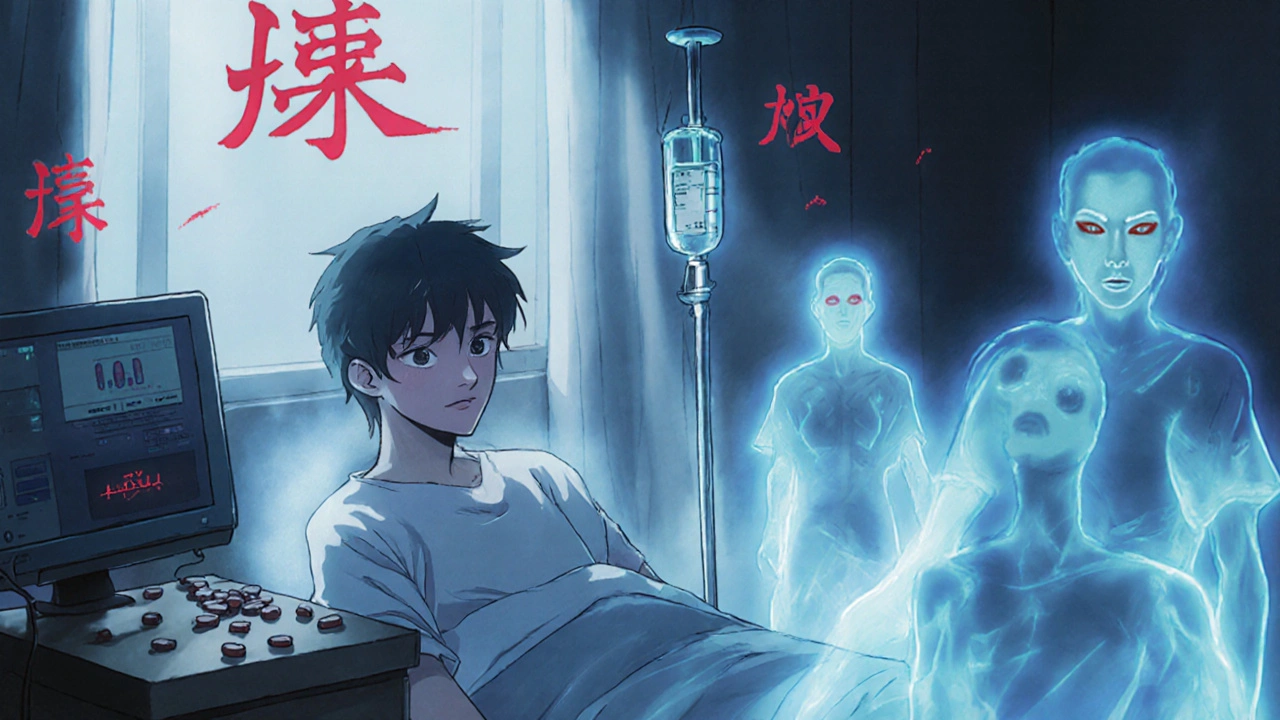
When high-dose corticosteroids like prednisone trigger steroid psychosis, a psychiatric condition caused by steroid use that includes hallucinations, delusions, and severe mood swings. Also known as corticosteroid-induced psychosis, it affects up to 6% of people on long-term, high-dose therapy, especially those with pre-existing mental health risks. This isn’t just anxiety or stress—it’s a real neurological reaction that needs targeted treatment. Many doctors turn to antipsychotics, medications designed to reduce psychotic symptoms by balancing brain chemicals like dopamine. Also known as neuroleptics, these drugs don’t cure the root cause, but they calm the mind enough for the body to recover.
Steroid psychosis usually shows up within weeks of starting high-dose steroids, and it’s more common in older adults or those with a history of depression, bipolar disorder, or previous psychotic episodes. The symptoms can be scary—seeing things that aren’t there, believing false ideas, or becoming extremely agitated. That’s where antipsychotics come in. Risperidone and olanzapine are often first choices because they’re effective at low doses and have fewer movement-related side effects than older drugs like haloperidol. But not all antipsychotics are equal. Some, like ziprasidone, carry heart rhythm risks that could be dangerous if the patient is already on steroids that affect electrolytes. The goal isn’t to sedate the patient, but to restore clarity so they can tolerate steroid tapering or switch to a safer treatment.
Doctors don’t just pick a drug at random. They look at the patient’s age, heart health, other medications, and how fast the psychosis came on. Some cases improve just by lowering the steroid dose—but if symptoms are severe, antipsychotics are needed fast. And while these drugs help, they’re not a long-term fix. Once the steroids are reduced and the brain resets, most people stop the antipsychotics without relapse. But missing the signs can lead to hospitalization, self-harm, or dangerous behavior. That’s why knowing which antipsychotics work best, how quickly they kick in, and what side effects to watch for matters more than ever.
Below, you’ll find real-world insights from posts that dig into how these medications affect mental health over time, what side effects to track, and how they compare to other treatments. You’ll see what works for patients, what doesn’t, and why some doctors hesitate to prescribe certain drugs. This isn’t theory—it’s what’s happening in clinics and homes right now.