Loperamide Abuse: Hidden Dangers of OTC Antidiarrheals and How to Spot the Warning Signs

Most people think of loperamide as just another medicine for a bad stomach. You grab a bottle of Imodium A-D at the pharmacy, pop a couple of pills, and within hours, the cramps and urgency fade. It’s safe, right? Over-the-counter means harmless. But what if I told you that taking just 10 or 20 pills - not for diarrhea, but to get high or ease opioid withdrawal - could stop your heart?
How a Common Diarrhea Medicine Became a Hidden Opioid
Loperamide was designed to be different from other opioid drugs. When it was first approved in the 1970s, the goal was simple: give people relief from diarrhea without the risk of addiction. And for decades, it worked. At the right dose - 2 to 4 mg at a time, no more than 8 mg in a day - loperamide stays in your gut. It binds to opioid receptors there, slowing down bowel movements, but doesn’t cross into your brain. That’s thanks to a natural defense system called P-glycoprotein, which acts like a bouncer, kicking loperamide out before it can reach your central nervous system.
But when someone takes 50, 100, even 400 mg a day - that’s 50 to 200 times the recommended dose - the bouncer gets overwhelmed. The system saturates. Loperamide slips through. And suddenly, it starts acting like heroin or oxycodone in the brain. Not as powerfully. Not with the same rush. But enough to make someone feel numb, calm, or even slightly euphoric. That’s why people with opioid addiction started turning to it. It’s cheap. It’s legal. And you can buy it next to the gum and candy at any pharmacy.
The Real Danger Isn’t the High - It’s Your Heart
Here’s the brutal truth: loperamide doesn’t give you a good high. It gives you a bad heart. At abusive doses, it doesn’t just affect your brain - it messes with your heart’s electrical system. It blocks potassium channels in heart cells, especially the hERG channel. That’s the same channel targeted by drugs like methadone and certain antibiotics that carry black box warnings for sudden death.
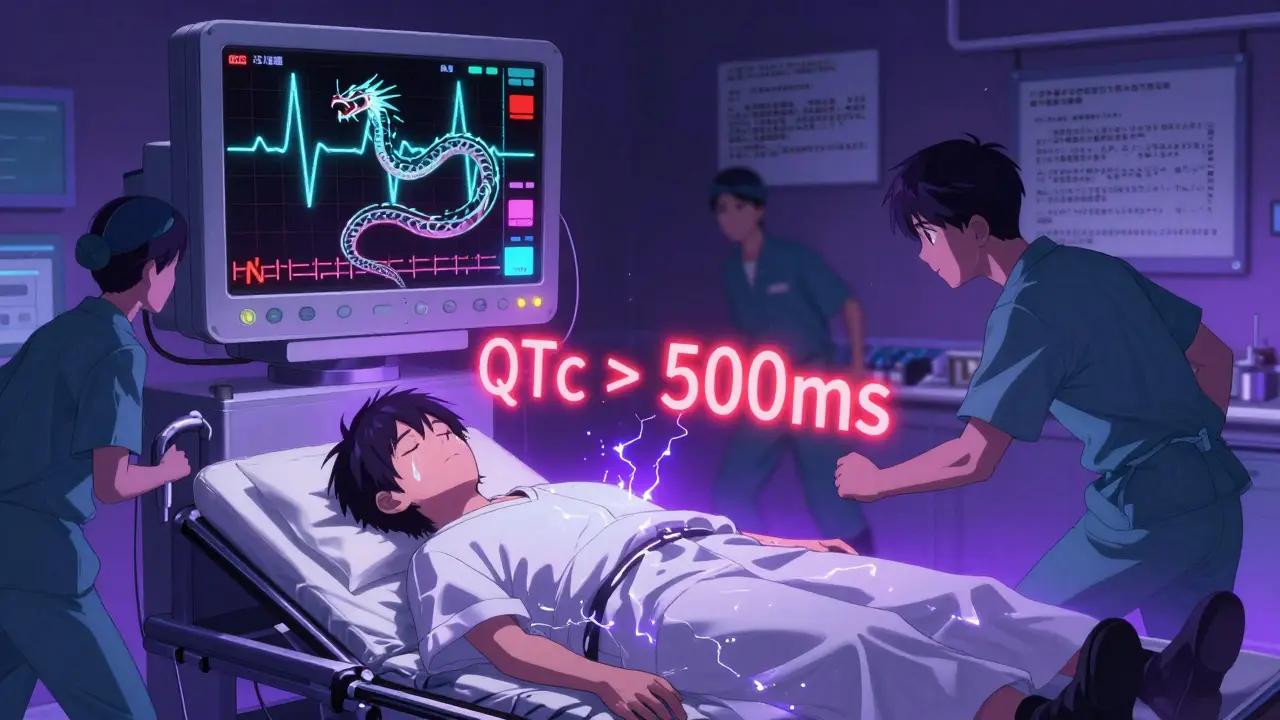
What happens? Your heart’s rhythm gets out of sync. The QT interval on an ECG stretches longer than it should. That’s a red flag. If it gets long enough, you can develop torsades de pointes - a type of dangerous, twisting heart rhythm that can turn into cardiac arrest. You won’t feel it coming. No warning buzz. No dizziness. Just sudden collapse. And sometimes, death.
The FDA reviewed 48 serious cases of loperamide-related heart problems. More than half happened after 2010. In one case, a 32-year-old man took 80 mg a day to manage opioid withdrawal. He ended up in the ER with polymorphic ventricular tachycardia. His QTc was over 500 ms - more than double the safe limit. He survived. Others didn’t. Between 2011 and 2020, at least 17 deaths were directly tied to loperamide overdose.
Warning Signs No One Talks About
If someone you know is using loperamide in large amounts, they might not look like a drug addict. They might just seem tired, quiet, or overly focused on staying “regular.” But there are clear red flags:
- Buying multiple bottles of Imodium at once - sometimes dozens at a time
- Using loperamide with other drugs like diphenhydramine (Benadryl), cimetidine (Tagamet), or quinidine to boost absorption
- Complaining of chest pain, palpitations, or fainting spells - especially after taking more than 4 pills
- Extreme constipation, bloating, or nausea that doesn’t go away
- History of opioid use disorder, or being in recovery and suddenly secretive about medications
These aren’t just side effects. They’re signs of toxicity. And they’re often missed. Emergency rooms see patients with unexplained cardiac arrest and assume it’s a heart attack. They don’t think of loperamide. But if the person has a history of drug use, or if their ECG shows prolonged QT or QRS intervals, it should be the first thing checked.
Why People Risk It - And Why It’s a Trap
Most people who abuse loperamide aren’t looking to get high. They’re trying to survive withdrawal. Opioid withdrawal is brutal: shaking, sweating, nausea, muscle aches, anxiety, insomnia. Some don’t have access to methadone or buprenorphine. Others don’t want to go to a clinic. So they turn to loperamide. Reddit threads from r/opioidrecovery are full of posts like: “Tried 50mg Imodium to help with withdrawal… wound up in ER with chest pains.”
But here’s the trap: loperamide doesn’t fix withdrawal. It masks it - and makes it deadlier. It doesn’t reduce cravings like buprenorphine does. It doesn’t stabilize brain chemistry. It just dumps your system with a toxin that can kill you. And because it’s so easy to get, people keep trying higher doses. Each time, the risk goes up. The body doesn’t build tolerance to the heart damage - only to the weak, fleeting effects.

What’s Being Done - And What’s Still Missing
In 2016, the FDA issued a safety alert. In 2019, manufacturers started putting loperamide in single-dose blister packs if the package contains more than 45 mg total. Sales dropped 12% after that. But people still buy it online in bulk. Some order 500 pills at a time. Others crush pills and mix them with liquids to bypass the slow-release coating.
Doctors now know to ask about loperamide use in patients with unexplained heart rhythm issues. Toxicology screens don’t detect loperamide - you need a specific blood test. And naloxone, the opioid overdose reversal drug, doesn’t fully work on loperamide. It might help with breathing or sedation, but it won’t fix the heart damage.
The real solution? Education. Not restriction. The FDA decided to keep loperamide over-the-counter because it’s still lifesaving for people with real diarrhea - like travelers, kids with stomach bugs, or cancer patients. But they added stronger warnings on packaging. SAMHSA now includes loperamide in its opioid misuse prevention materials. Pharmacies in Australia and the U.S. are training staff to recognize suspicious purchases.
If You or Someone You Know Is Using Loperamide Too Much
Stop. Immediately. Don’t wait for symptoms. If someone is taking more than 8 mg a day - even if they say they’re just “trying to feel better” - it’s abuse. And it’s dangerous.
Here’s what to do:
- Stop all loperamide use. No more pills.
- Get an ECG. Even if they feel fine. A prolonged QT interval can be silent.
- Don’t try to quit cold turkey if they’re also using opioids. Withdrawal can get worse. Seek medical help.
- If they’re having chest pain, dizziness, or fainting - call emergency services. Tell them loperamide was used.
- For long-term recovery, connect with a substance use counselor. Medications like buprenorphine are safe, effective, and legally available.
There’s no shame in asking for help. But there’s huge risk in thinking loperamide is harmless because it’s sold next to aspirin. It’s not. It’s a powerful drug - and when misused, it’s a silent killer.
Can you overdose on loperamide even if you’re not trying to get high?
Yes. Many people take more than the recommended dose because they think more pills will stop diarrhea faster. But exceeding 8 mg a day increases the risk of heart rhythm problems. Even 12-16 mg can be dangerous. The body doesn’t need more than the standard dose to work - extra amounts just raise toxicity without extra benefit.
Does loperamide show up on a standard drug test?
No. Most workplace or probation drug tests screen for common opioids like morphine, codeine, or oxycodone. Loperamide is not detected in these tests. You need a specialized blood test to find it. That’s why abuse often goes unnoticed - until someone ends up in the ER with a heart problem.
Is loperamide safer than methadone or buprenorphine for opioid withdrawal?
No. Methadone and buprenorphine are FDA-approved for opioid use disorder and are given under medical supervision. They’re carefully dosed to reduce cravings and withdrawal without causing heart damage. Loperamide has no medical approval for this use. It’s unpredictable, carries high cardiac risk, and offers no real therapeutic benefit for addiction recovery.
What should I do if I suspect someone is abusing loperamide?
Don’t confront them with judgment. Ask if they’re feeling okay, and gently suggest they see a doctor - especially if they’ve had chest pain, dizziness, or irregular heartbeat. Offer to help them find a substance use counselor. Many people don’t realize how dangerous it is until they’re told by a professional. Resources like SAMHSA’s helpline (1-800-662-HELP) can connect them to free, confidential support.
Can loperamide abuse cause long-term heart damage?
In some cases, yes. Repeated episodes of torsades de pointes or cardiac arrest can scar the heart muscle or damage its electrical system permanently. Even if someone survives, they may need a pacemaker or defibrillator later in life. The damage isn’t always reversible - especially if treatment is delayed.
Are there any safe alternatives to loperamide for diarrhea?
Yes. For most cases of acute diarrhea, hydration and time are the best treatments. Oral rehydration solutions (like Pedialyte or WHO-ORS) replace lost fluids and electrolytes. Probiotics, like Lactobacillus rhamnosus GG, have been shown to shorten diarrhea duration. Avoid anti-diarrheals unless symptoms are severe or persistent - and never exceed the label dose.
If you’ve ever thought loperamide was just a harmless fix for a stomach bug - think again. It’s one of the most dangerous drugs you can buy without a prescription. And the people most at risk aren’t the ones chasing a high. They’re the ones trying to survive.


Wow-this is terrifying. I had no idea loperamide could do this to your heart. I’ve seen people in my town buy entire boxes of Imodium after their opioid rehab, thinking it’s a ‘natural’ fix. But the fact that it blocks hERG channels? That’s straight-up pharmacological suicide. I’m going to print this out and leave it at the pharmacy counter.
This needs to be on every pharmacy shelf. Like, right next to the painkillers. I work in ER and we’ve had two cases this year alone-both young guys, 20s, no history of heart issues. One died. The other got a pacemaker. They didn’t even know they were poisoning themselves. Stop treating OTC like ‘safe.’ It’s not. If you’re using this for withdrawal, you need real help-not a pharmacy aisle.
It’s wild how we treat some drugs like candy because they’re legal. We panic about fentanyl, but ignore the silent killer on the next aisle. I used to take 4 pills when I had food poisoning-never thought twice. Now I feel guilty. This article didn’t just inform me-it changed how I see everyday medicine.
The systemic failure here isn’t just individual misuse-it’s institutional ignorance. Pharmacists aren’t trained to recognize patterns. Medical schools don’t teach loperamide toxicity in their opioid modules. Insurance doesn’t cover the specialized blood tests. And the FDA’s blister-pack solution? A Band-Aid on a hemorrhage. We need mandatory screening protocols, public health campaigns, and real access to buprenorphine-not more warnings on bottles that no one reads.
Let us be unequivocal: the commodification of suffering has reached its nadir. Loperamide, a pharmacological artifact designed for gastrointestinal palliation, has been perverted into a pseudo-therapeutic opiate surrogate by a population bereft of access to evidence-based care. The P-glycoprotein saturation phenomenon is not an accident-it is the inevitable consequence of a healthcare infrastructure that abdicates its duty to the marginalized. One cannot blame the victim when the system has engineered the trap.
Did you know that Big Pharma knew about this for decades? They suppressed the data. The same people who pushed OxyContin are the ones who made sure loperamide stayed OTC. Why? Because it’s cheaper than methadone. And if people die? Well, that’s just the cost of capitalism. I saw a Reddit thread where someone said they bought 500 pills from India. That’s not coincidence-that’s a supply chain. Someone’s profiting off your death.
My cousin did this. Took 120mg over three days to get through withdrawal. Said it ‘calmed the storm.’ He didn’t collapse-he just got really quiet. Then he started having panic attacks every time his heart skipped. He’s in therapy now. Still scared to even hold a pill bottle. This isn’t just about overdoses. It’s about the quiet, slow unraveling. If you’re reading this and you’ve ever taken more than 8mg… please, just talk to someone. You’re not alone.
lol so basically imodium is the new fentanyl? i mean… its just a pill right? like… chill. i took 20 once and felt fine. prob just vibes. 🤷♀️