How Generic Medications Save Thousands on Healthcare Costs

When you pick up a prescription, you might see two options: the familiar brand-name pill in colorful packaging, or a plain white tablet with a generic label. Most people assume the brand is better. But here’s the truth: generic medications work just as well-and cost a fraction of the price.
In 2022, Americans saved $408 billion by choosing generics over brand-name drugs. That’s not a guess. That’s from IQVIA’s official report. Over the past decade, generics and biosimilars have saved the U.S. healthcare system nearly $3 trillion. And yet, many people still pay more than they need to-because they don’t know how much they’re overpaying.
Why Generics Cost So Much Less
Generic drugs aren’t cheaper because they’re lower quality. They’re cheaper because they don’t need to repeat the billion-dollar clinical trials that brand-name companies run to get FDA approval. Once a patent expires, other manufacturers can produce the same drug using the same active ingredient. The FDA requires generics to be bioequivalent: meaning they deliver the same amount of medicine into your bloodstream at the same rate as the brand. The standard? 80% to 125% similarity in absorption. That’s not a loophole. That’s science.
Here’s what that looks like in your pocket: the average copay for a brand-name drug is $56.12. For a generic? $6.16. That’s more than nine times cheaper. In fact, 93% of generic prescriptions cost under $20. Only 59% of brand-name prescriptions do. You’re not getting less medicine-you’re paying less for the same medicine.
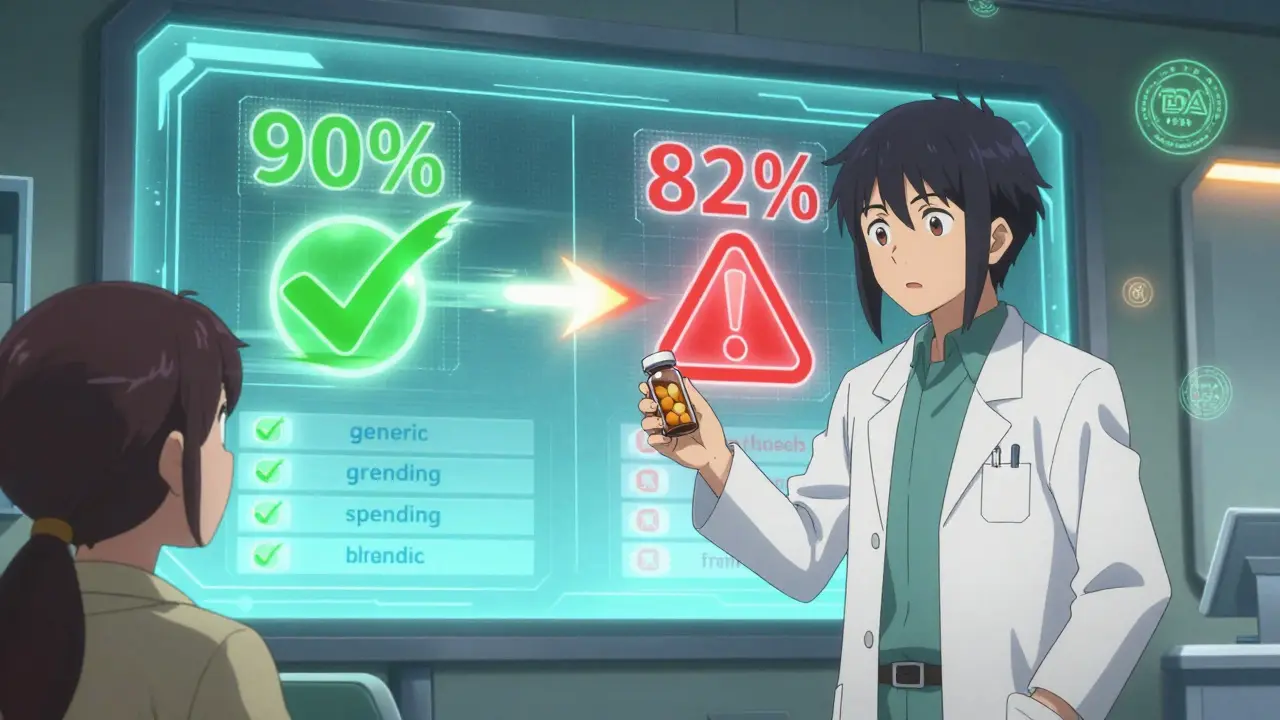
Generics Dominate Prescriptions-But Not Costs
It’s a simple math trick: generics make up 90% of all prescriptions filled in the U.S. But they account for only 1.5% of total drug spending. Meanwhile, brand-name drugs, which make up just 10% of prescriptions, take up 82% of the money spent on prescriptions. That’s not a typo. It’s a system where a small number of expensive drugs drive most of the cost.
Take statins, for example. Almost every patient on cholesterol medication gets a generic like atorvastatin or rosuvastatin. Those generics saved billions. But look at drugs for epilepsy or thyroid conditions. Even though generics exist, doctors sometimes stick with brands because of outdated fears. In reality, 98% of FDA-approved generics are rated AB-meaning they’re therapeutically equivalent. If your doctor says a generic won’t work the same, ask them to show you the data.
Therapeutic Substitution: The Hidden Savings
Most people think savings come from swapping a brand for its generic. But the real money is in swapping one generic for another.
A 2022 study from Johns Hopkins looked at the top 1,000 generic drugs in Colorado. They found 45 high-cost generics that had cheaper alternatives with the same effect. One example: a generic version of a thyroid medication was priced at $120 a month. A different generic, with the same active ingredient but a different dosage form, cost $6. That’s a 95% drop. In 62% of cases, the savings came from switching dosage forms-like going from a tablet to a capsule, or changing the strength. These aren’t experimental swaps. They’re approved, safe, and often overlooked.
Doctors rarely think to ask: "Is there a cheaper version of this generic?" But pharmacists do. If you’re paying more than $20 for a generic, ask your pharmacist: "Is there another version of this drug that costs less?" They have access to formularies that show price differences between manufacturers. It’s not magic. It’s just knowledge.
Who’s Saving the Most?
Medicare patients filled 91% of their prescriptions with generics in 2022. That’s great-but 41% still struggled to afford them. Why? Because even though the drug costs $5, your copay might be $15. That’s because insurance plans often set high copays to push patients toward cheaper options. But if the generic is already cheap, why are you still paying so much?
The Inflation Reduction Act of 2023 capped out-of-pocket drug costs for Medicare Part D at $2,000 a year. That’s a big win. But it doesn’t fix the problem for people with private insurance. If your plan has a $50 copay for a $7 generic, you’re being overcharged. Call your insurer. Ask why. And if they can’t explain it, ask your pharmacist to help you find a lower-cost alternative.
What About Safety? Are Generics Really the Same?
Some people worry that generics are made in cheaper factories overseas. That’s true for some-but so are brand-name drugs. The FDA inspects all manufacturing facilities, whether they make brand or generic. In fact, many brand-name companies make their own generics after the patent expires.
There are rare cases where people report issues with generics-especially with drugs that have a narrow therapeutic index, like levothyroxine or warfarin. But these are exceptions. A 2023 Drugs.com survey of 240 people found only 15% reported problems. Most of those were due to switching between different generic manufacturers, not because generics are inherently less effective.
The FDA requires strict testing. If a generic doesn’t work the same way, it doesn’t get approved. If you’ve had a bad experience, it’s worth talking to your doctor. But don’t assume the problem is the generic. It might be the specific manufacturer. Try switching to a different brand of the same generic drug. Often, that fixes it.
Why Don’t More People Use Generics?
It’s not ignorance. It’s marketing.
Brand-name companies spend billions on ads that make you believe their drug is superior. They pay doctors to recommend their version. They create patient assistance programs that make their drug seem affordable-even though it’s not. Meanwhile, generics have no marketing budget. They’re silent. But they’re everywhere.
Consumer Reports surveyed 1,500 adults in 2022. 78% said they actively ask for generics. 63% said they’d switch pharmacies to get a better price. That’s power. You don’t need to be a doctor to make this choice. You just need to ask.

What You Can Do Today
Here’s how to start saving right now:
- Check your last prescription. Is it brand or generic? If it’s brand, ask your doctor: "Is there a generic version?"
- If it’s already generic, ask your pharmacist: "Is there a cheaper version of this generic?"
- Use the FDA’s Orange Book online (or ask your pharmacist to check it) to see which generics are rated AB-therapeutically equivalent.
- If your copay is over $20 for a generic, call your insurance company. Ask why.
- Don’t assume your current pharmacy has the lowest price. Compare prices at Walmart, Costco, or CVS. Many offer $4 generic lists.
These aren’t complicated steps. They’re simple, practical actions that can save you hundreds-or even thousands-each year.
The Bigger Picture
Generics aren’t a magic fix for America’s high drug prices. The U.S. still pays 2.78 times more for prescriptions than other wealthy countries. But without generics, the cost would be unbearable.
Right now, the FDA approves over 800 new generics every year. Teva, Viatris, and Amneal are the top manufacturers. They’re not flashy. They don’t run Super Bowl ads. But they’re the reason millions of people can afford their medications.
The real threat isn’t generics. It’s delays. Brand companies file dozens of patents to block generics from entering the market. The FTC found that, on average, a brand-name drug gets hit with 17.5 patents to extend its monopoly. That’s not innovation. That’s obstruction.
But you have power. Every time you choose a generic, you’re voting against inflated prices. You’re helping keep costs down for everyone. And you’re putting money back in your own pocket.
Are generic medications as effective as brand-name drugs?
Yes. The FDA requires generics to have the same active ingredient, strength, dosage form, and bioequivalence as the brand-name version. This means they work the same way in your body. Over 98% of FDA-approved generics are rated "AB," meaning they’re therapeutically equivalent. Millions of people use generics every day with the same results as brand-name drugs.
Why are generics so much cheaper?
Generics don’t have to repeat expensive clinical trials because they’re based on drugs already proven safe and effective. The approval process is faster and cheaper, which lets manufacturers sell them at lower prices. Brand-name companies recoup their R&D costs through high prices during their patent period. Once that ends, competition drives prices down-often by 80-85% in the first year.
Can I switch from a brand to a generic without my doctor’s approval?
In 49 states, pharmacists can automatically substitute a generic for a brand-name drug unless the doctor writes "Dispense as Written" on the prescription. In New York, the doctor must specifically indicate that substitution is allowed. If you’re unsure, ask your pharmacist. They’re trained to handle substitutions safely.
What if I have a bad reaction to a generic?
While rare, some people report differences when switching between generic manufacturers-even for the same drug. This can happen due to inactive ingredients or slight variations in absorption. If you notice changes in how you feel, talk to your doctor. You can often switch to a different generic brand or return to the brand if needed. Keep a record of which manufacturer you’re using so you can track any patterns.
Do generics have the same side effects as brand-name drugs?
Yes. Since generics contain the same active ingredient and work the same way in your body, their side effects are identical. Any differences you notice are likely due to inactive ingredients (like fillers or dyes), which can affect how quickly the drug is absorbed. These are usually minor and don’t change the drug’s safety profile.
How can I find the cheapest version of my generic medication?
Ask your pharmacist to check the FDA’s Orange Book for therapeutic equivalents. Then compare prices at different pharmacies-Walmart, Costco, and CVS often have $4 or $10 generic lists. You can also use apps like GoodRx to compare prices across local pharmacies. Sometimes, switching from one generic manufacturer to another can cut your cost in half.
Are biosimilars the same as generics?
No. Biosimilars are similar to brand-name biologic drugs (like those for arthritis or cancer), but they’re made from living cells, not chemicals. They’re more complex to produce and aren’t as cheap as traditional generics. Still, they’re saving billions and are becoming more common. The FDA has approved over 40 biosimilars as of 2023, and their use is growing.
Final Thought
You don’t need to be an expert to save money on prescriptions. You just need to ask the right questions. Generics aren’t a compromise. They’re the smart choice. And if you’re paying more than you should, it’s not because you’re missing something. It’s because the system is designed to make you think you are.

Let’s be clear: the FDA’s bioequivalence standard of 80% to 125% isn’t science-it’s a loophole dressed up as regulation. If your drug’s absorption varies by 45% depending on the manufacturer, that’s not equivalent. That’s gambling with your health. And don’t get me started on the foreign manufacturing facilities that aren’t inspected as rigorously as they claim. I’ve seen patients crash after switching generics. It’s not anecdotal. It’s systemic.
i just switched my atorvastatin from the $12 brand to the $3 generic at walmart and my cholesterol dropped even more. weird right? but my pharmacist said the inactive ingredients can affect how fast it hits the bloodstream, so maybe the one i got is just better absorbed. also, they have like 5 different versions of the same drug and the prices vary by like 300%. just ask for the cheapest ab-rated one. no one tells you this.
Generics are fine unless you’re one of those people who actually needs precision. I had a friend on warfarin who went from one generic to another and ended up in the ER. The doctor said it was the filler. The generic makers don’t even have to list the fillers. That’s not transparency. That’s negligence. And now the FDA lets them swap manufacturers without telling you. You’re basically a lab rat.
While the article presents a compelling narrative regarding the cost-efficiency of generic medications, it conspicuously omits the structural power dynamics inherent in pharmaceutical patent law and the regulatory capture that enables brand-name manufacturers to extend monopolies through evergreening tactics. The notion that 90% of prescriptions being filled by generics equates to systemic success is a statistical illusion; the true metric lies in the percentage of patients who are financially liberated as a result. Moreover, the FDA’s bioequivalence thresholds, while mathematically defensible, fail to account for interindividual pharmacokinetic variability, particularly among geriatric and pediatric populations. The suggestion that patients should simply ‘ask their pharmacist’ for a cheaper alternative presumes universal access to informed pharmaceutical counsel, a privilege not extended to rural, low-income, or underinsured communities. Furthermore, the implicit endorsement of therapeutic substitution ignores the fact that many generic manufacturers operate under minimal quality control standards, with recent FDA warning letters citing contamination, inconsistent dissolution rates, and inadequate stability testing in over 30% of inspected facilities. The real savings, then, are not in the pill-but in the erosion of patient autonomy under the guise of fiscal responsibility.
my mom switched from brand name levothyroxine to a generic and started having panic attacks. she went back and the symptoms stopped. i asked the pharmacist and they said it happens sometimes because of the fillers. so now she gets the same generic every time and writes down the manufacturer. it’s not about brand vs generic-it’s about consistency. if you’re on something sensitive, stick with one maker. and yes, the $4 list at walmart is real. i got my blood pressure med for $1.25 last month. 🙌
Just got my metformin for $3.50. No drama. No panic. Just saved $50 a month. Thanks for the reminder.
How delightful that we’re all supposed to be thrilled that our lives are now governed by pharmaceutical cost-cutting measures disguised as ‘smart choices.’ You don’t need a PhD to see this: the system doesn’t want you healthy. It wants you compliant. Generics are the opiate of the masses-cheap, abundant, and designed to make you feel like you’re winning while the real players-Big Pharma, insurance middlemen, pharmacy benefit managers-collect their 82% slice of the pie. And now you’re supposed to be grateful you’re not paying $60 for a pill you could’ve gotten for $6? That’s not empowerment. That’s psychological surrender dressed in a lab coat.
lol so the FDA inspects all factories right? sure. and the moon landing was real too. did you know that 70% of generic drugs are made in india and china? and the FDA sends inspectors once every 10 years? and when they find contamination? they just say 'we trust you to fix it.' meanwhile, my cousin's kid had a seizure after switching generics. the hospital said 'it's probably the filler.' but no one ever tells you which filler. it's all a scam. they want you docile. cheap meds. quiet patients. no questions. just take the white pill and don't complain.
my pharmacist just told me that the generic for my antidepressant is $1.50 at costco but $18 at my usual place. i switched and didn’t even notice a difference. also, i asked if there was another version and they showed me three with the same active ingredient. i picked the cheapest. i feel like this should be common knowledge but no one talks about it. thanks for the post-this is the kind of info that actually helps.