Hidden Dangers of Undiagnosed Allergic Disorders: Risks You Can’t Ignore

Undiagnosed allergic disorder is a medical condition where the immune system reacts to a harmless substance, yet the patient never receives a formal diagnosis. Without proper identification, the reaction can progress unnoticed, turning mild irritation into life‑threatening complications. Most people think allergies are just sneezes or rashes, but the reality is far grimmer. When the body’s alarm system stays silent, inflammation builds, organ function declines, and everyday life becomes a minefield of hidden triggers.
Why Some Allergies Fly Under the Radar
Several factors keep allergies hidden:
- Non‑classic symptoms: Fatigue, brain fog, or joint pain often get blamed on stress or aging.
- Overlap with other diseases: Conditions like asthma or eczema may mask the underlying allergy.
- Lack of testing: Primary care visits rarely include comprehensive IgE panels unless the patient reports obvious reactions.
These gaps mean patients and doctors miss the warning signs until damage is done.
Hidden Dangers: From Mild Irritation to Severe Outcomes
Undiagnosed allergies can unleash a cascade of problems:
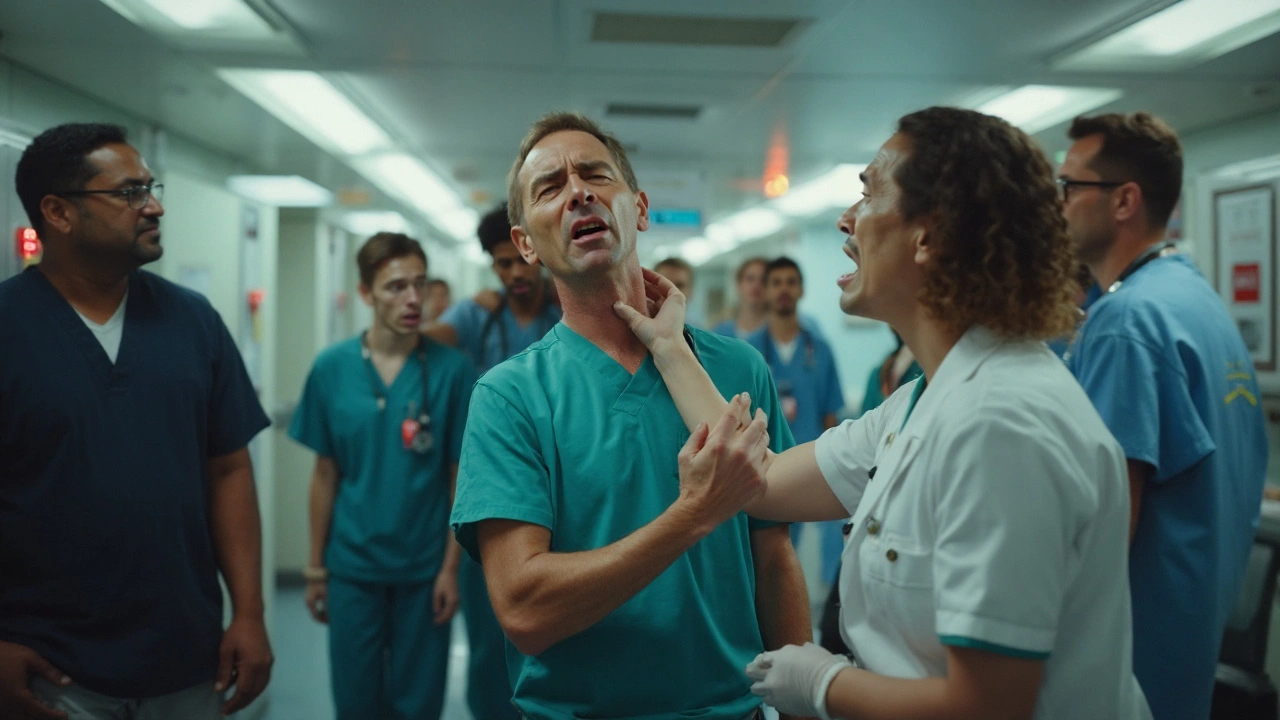
- Anaphylaxis - A sudden, systemic reaction that can cause airway closure, shock, or cardiac arrest. Without prior knowledge, there’s no epinephrine auto‑injector on hand.
- Chronic inflammation - Persistent activation of mast cells releases histamine, cytokines, and leukotrienes, damaging blood vessels and tissues over years.
- Organ‑specific injury - Food allergens can erode the gut lining, leading to leaky gut syndrome, malabsorption, and even eosinophilic esophagitis.
- Misdiagnosis - Symptoms like chronic cough or sinus pressure often get labeled as infections, resulting in unnecessary antibiotics.
- Mental health strain - Unknown triggers cause anxiety, depression, and reduced quality of life.
- Economic burden - Repeated ER visits, missed workdays, and costly specialist referrals add up quickly.
Common Undiagnosed Allergic Disorders
The following conditions often slip through standard screening:
- Food allergy - Especially to nuts, shellfish, or hidden additives in processed foods.
- Allergic rhinitis - Sneezing, congestion, and itchy eyes that many dismiss as “just a cold.”
- Atopic dermatitis - Chronic skin eczema that can be driven by invisible food or environmental allergens.
- Asthma - Exercise‑induced or occupational asthma often hidden behind “shortness of breath.”
- Mast cell activation syndrome (MCAS) - Flare‑ups affecting multiple organ systems, frequently misread as auto‑immune flare.
How to Spot the Silent Signals
Pay attention to patterns that don’t fit typical illnesses:
- Temporal clustering: Symptoms appear after the same meals, weather changes, or exposure to specific fabrics.
- Multi‑system involvement: Simultaneous skin, respiratory, and gastrointestinal complaints.
- Family history: Allergies often run in families; a parent’s hay fever or child’s peanut allergy raises suspicion.
- Response to antihistamines: Temporary relief after over‑the‑counter meds hints at an allergic component.
Diagnostic Toolbox: From Simple Tests to Advanced Panels
Once suspicion builds, clinicians can deploy a range of tools:
- Skin prick test (SPT) - Small amounts of allergens placed on the forearm; a wheal indicates IgE‑mediated sensitivity.
- Specific IgE blood test - Measures antibody levels against a panel of foods, pollens, and chemicals.
- Oral food challenge - Gold‑standard supervised ingestion to confirm or rule out food allergy.
- Component‑resolved diagnostics - Breaks down allergens into protein families, clarifying cross‑reactivity.
- Basophil activation test - Emerging lab method useful for complex cases like MCAS.
Choosing the right test depends on symptom severity, suspected trigger, and patient age.
Comparison: Undiagnosed vs. Diagnosed Allergic Disorders
| Aspect | Undiagnosed | Diagnosed |
|---|---|---|
| Symptom clarity | Vague, multi‑system | Specific, trigger‑linked |
| Risk of severe reaction | High - no emergency plan | Managed - epinephrine available |
| Medical costs (annual) | AU$3,200≈multiple ER visits | AU$1,200≈targeted therapy |
| Quality of life score | 52/100 (lower) | 78/100 (higher) |
| Long‑term complications | Chronic inflammation, organ damage | Reduced risk with avoidance |
The numbers come from recent Australian public‑health surveys and peer‑reviewed cohort studies (2023). They underline why early detection matters.
Managing the Hidden Threat
Once an allergy is identified, a three‑pronged approach keeps risks low:
- Avoidance strategy: Read labels, adopt a “clean kitchen” habit, and use air‑purifiers for environmental triggers.
- Medication plan: Keep antihistamines and, when indicated, a prescribed epinephrine auto‑injector on hand.
- Follow‑up monitoring: Annual reassessment with an allergist to track new sensitivities and adjust avoidance.
For conditions like MCAS, a low‑histamine diet paired with mast‑cell stabilizers (e.g., cromolyn) can dramatically reduce flare‑ups.
Related Concepts and Next Steps
Understanding undiagnosed allergies opens doors to broader topics:
- Gut‑immune axis: How chronic intestinal inflammation fuels systemic allergy responses.
- Precision medicine: Using genetic profiling to predict allergy susceptibility.
- Environmental health: The role of indoor pollutants and climate change in rising allergy rates.
Readers keen on digging deeper might explore "Allergy Immunotherapy Advances" or "The Impact of Climate on Seasonal Rhinitis" as logical next reads.
Quick Checklist for Self‑Assessment
- Do you experience recurring symptoms after certain foods, scents, or weather changes?
- Has an over‑the‑counter antihistamine ever helped?
- Is there a family history of asthma, eczema, or hay fever?
- Do you find yourself visiting the ER for unexplained breathing issues?
- Are you comfortable discussing a full allergy work‑up with your GP?
If you answered “yes” to three or more, schedule a consultation with an allergist. Early detection can prevent the hidden dangers outlined above.
Frequently Asked Questions
What are the most common signs of an undiagnosed food allergy?
Look for recurring stomach cramps, hives, or sudden fatigue after meals, especially with nuts, shellfish, or processed foods. Symptoms often appear 30minutes to a few hours post‑ingestion and may be dismissed as indigestion.
Can adult‑onset allergies be just as dangerous as childhood ones?
Absolutely. Adults can develop IgE‑mediated allergies to foods or inhalants that trigger anaphylaxis. Because they often lack a prior allergy history, they’re less likely to carry emergency medication, raising the risk of severe outcomes.
How reliable are over‑the‑counter antihistamines for diagnosing allergies?
They’re a useful screening tool. If symptoms improve within an hour of taking a non‑sedating antihistamine (e.g., cetirizine), an allergic component is likely. However, antihistamines do not replace formal skin or blood testing.
What is Mast Cell Activation Syndrome and why is it often missed?
MCAS is a disorder where mast cells release mediators without a classic allergen trigger, causing flushing, abdominal pain, and brain fog. Standard allergy panels test only IgE, so MCAS can slip through unless a basophil activation test or tryptase measurement is ordered.
Does insurance typically cover allergy testing in Australia?
Most private health funds provide rebates for skin prick and specific IgE tests when prescribed by a specialist. Public hospitals may offer testing on a referral basis for high‑risk patients, though waiting times can be long.


Wow, this is a wake‑up call for anyone ignoring their weird symptoms! 😱
I read this and think it’s kinda obvious that people skip allergy tests cause doctors are busy. But still, many dont realize that a simple skin prick can save a life. You should ask your gp for a full IgE panel if you have any weird rashes.
Even a tiny reaction might be a sign of something bigger.
It is imperative to recognize that the phenomenon of undiagnosed allergic disorders is not merely a clinical curiosity but a public‑health exigency. The literature consistently demonstrates that delayed identification of IgE‑mediated sensitivities correlates with increased morbidity and healthcare expenditure. Furthermore, the pathophysiological cascade initiated by uncontrolled mast‑cell degranulation entails cytokine release, vascular permeability, and tissue remodeling, all of which predispose to chronic organ dysfunction. One must also contend with the insidious nature of non‑classic manifestations-fatigue, cognitive fog, and arthralgia-frequently misattributed to psychosomatic origins. The epidemiological data from Australian cohorts underscore a stark disparity: an annual cost burden exceeding AU$3,000 for the undiagnosed versus roughly a third of that for those under specialist care. Moreover, quality‑of‑life indices reveal a precipitous decline in the former group, echoing findings from European allergy registries. It is therefore not a hyperbolic assertion to claim that systematic screening, particularly in high‑risk populations, constitutes a preventive strategy of profound socioeconomic relevance. The diagnostic armamentarium, ranging from skin‑prick testing to component‑resolved profiling, offers granularity sufficient to delineate true sensitizations from cross‑reactive epitopes. Equally important is the burgeoning role of basophil activation assays in elucidating atypical presentations such as MCAS, wherein traditional IgE assays may yield false‑negative results. Clinical prudence dictates that any patient exhibiting multi‑systemic symptoms with temporal clustering should be evaluated with the full spectrum of available modalities. In practice, this translates to a collaborative model involving primary care physicians, allergists, and, when warranted, immunologists. The therapeutic algorithm, once an allergen is identified, hinges upon avoidance, pharmacologic prophylaxis, and periodic reassessment to accommodate evolving sensitivities. Finally, the ethical imperative to educate patients about the hidden dangers of unrecognized allergies cannot be overstated; empowerment through knowledge remains the cornerstone of effective disease mitigation.
Contemplating the cascade you describe, one discerns a deeper philosophical lesson about the interplay between ignorance and vulnerability. The body, in its elegance, offers subtle signals, yet we habitually prioritize the tangible over the unseen. When the unnoticed triggers accumulate, the resultant disarray mirrors a society that dismisses marginal voices. Hence, vigilance is not merely a medical directive but an ethical one. By honoring the quiet warnings our physiology offers, we affirm a respect for the holistic self.
In light of the observations presented earlier, it becomes evident that a nuanced approach to allergic evaluation is warranted. The patient’s narrative should be foregrounded, allowing clinicians to map symptom clusters across temporal and environmental axes. While the skin prick test remains a cornerstone, its limitations necessitate adjunctive assays, particularly when faced with atypical presentations. Moreover, the psychosocial ramifications-ranging from anxiety to occupational impairment-must be integrated into the management plan. A multidisciplinary cohort, comprising allergists, nutritionists, and mental‑health professionals, can orchestrate a comprehensive strategy that transcends mere avoidance. Ultimately, the goal is not solely the abatement of acute episodes but the cultivation of a resilient, informed individual capable of navigating the allergen‑laden landscape of modern life.
The discourse surrounding hidden allergic threats often suffers from a paucity of longitudinal insight, yet the data presented compellingly illustrate the cumulative burden of neglect. When clinicians remain myopic, focusing exclusively on overt hypersensitivity, they inadvertently sanction a silent progression toward systemic inflammation. This oversight is not merely a clinical failing; it reflects a broader cultural tendency to marginalize subtler forms of suffering. By advocating for comprehensive screening protocols and fostering patient education, we can dismantle the inertia that perpetuates these hidden dangers. It is incumbent upon the medical community to champion proactive detection, thereby averting the cascade of complications that, as the evidence delineates, are both preventable and profoundly detrimental.